Pancreatic cancer is one of the most aggressive forms of cancer, often discovered at a late stage due to its subtle early symptoms. Many people wonder how is pancreatic cancer diagnosed, since early detection is key to improving survival rates. Understanding the process of diagnosis can help patients and families prepare for what to expect.
This article provides a comprehensive overview of pancreatic cancer, from its definition and types to the risk factors, symptoms, and medical procedures involved in diagnosis. We will also discuss treatment options, prevention strategies, prognosis, and recent research innovations that bring hope for better outcomes.
Definition and Overview
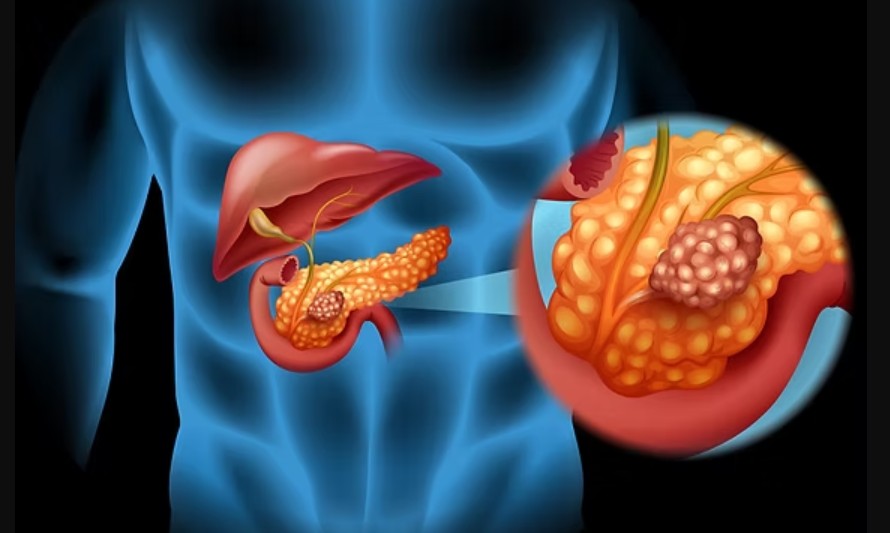
Pancreatic cancer occurs when malignant cells develop in the tissues of the pancreas, an organ located behind the stomach that plays an essential role in digestion and hormone production. Because the pancreas is deep inside the abdomen, tumors often go unnoticed until they reach advanced stages.
The disease is relatively rare compared to other cancers, but it is highly lethal due to its fast progression. Therefore, knowing how pancreatic cancer is diagnosed is critical to enabling timely treatment and improving the patient’s chances of survival.
Types of Pancreatic Cancer
Pancreatic cancer is classified into two main categories:
- Exocrine tumors – These account for about 90–95% of cases and include adenocarcinomas, which arise from the cells lining the pancreatic ducts.
- Endocrine tumors (neuroendocrine tumors) – Much less common, these tumors develop from hormone-producing cells and may grow more slowly.
The type of cancer influences both the diagnostic approach and the treatment plan.
Causes and Risk Factors
The exact cause of pancreatic cancer is still not fully understood, but several risk factors are known to increase the likelihood of developing the disease. These include:
- Genetics and family history – A family history of pancreatic cancer or certain genetic mutations.
- Lifestyle factors – Smoking, obesity, high-fat diets, and excessive alcohol consumption.
- Medical conditions – Chronic pancreatitis, diabetes, and certain inherited syndromes.
- Age and gender – Most cases occur in people over 60, with men slightly more affected than women.
Symptoms and Early Warning Signs
One of the challenges of pancreatic cancer is that early symptoms are often vague or absent. However, there are several warning signs that should not be ignored:
- Persistent abdominal or back pain
- Jaundice (yellowing of the skin and eyes)
- Unexplained weight loss and loss of appetite
- Fatigue and general weakness
- Digestive issues such as nausea, vomiting, or diarrhea
Recognizing these signs and seeking medical evaluation promptly is vital.
Diagnosis
So, how is pancreatic cancer diagnosed in clinical practice? Doctors use a combination of methods to confirm the disease:
- Medical history and physical examination – Evaluating symptoms, family history, and risk factors.
- Imaging tests – CT scans, MRI, PET scans, and ultrasound are used to detect abnormalities in the pancreas.
- Endoscopic procedures – Endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP) help visualize the pancreas more closely.
- Biopsy – The most definitive test, where a small tissue sample is taken and analyzed under a microscope.
- Blood tests – Tumor markers like CA 19-9 can support diagnosis but are not conclusive on their own.
A combination of these approaches ensures accuracy and helps determine the stage of cancer, which is crucial for treatment planning.
Treatment Options
Treatment for pancreatic cancer depends on the stage and type of the tumor. Common approaches include:
- Surgery – Such as the Whipple procedure, often for early-stage cases.
- Chemotherapy – To kill cancer cells and reduce tumor size.
- Radiation therapy – Often combined with chemotherapy.
- Targeted therapy and immunotherapy – Newer treatments that aim to attack cancer more precisely.
- Palliative care – To manage symptoms and improve quality of life in advanced cases.
Prevention and Lifestyle Recommendations
While pancreatic cancer cannot always be prevented, certain lifestyle choices can reduce risk:
- Quit smoking and avoid excessive alcohol consumption.
- Maintain a healthy diet rich in fruits, vegetables, and whole grains.
- Exercise regularly and maintain a healthy weight.
- Manage chronic conditions such as diabetes and pancreatitis.
- Get genetic counseling if you have a strong family history of pancreatic cancer.
Prognosis and Survival Rates
Pancreatic cancer has one of the lowest survival rates among major cancers, largely because it is diagnosed late. The overall 5-year survival rate is less than 12%, but outcomes improve significantly when the cancer is detected early and surgically removed. Factors such as tumor size, stage, type, and overall health influence prognosis.
Latest Research and Innovations
Research on pancreatic cancer is advancing rapidly. Scientists are exploring better imaging techniques, liquid biopsies, and genetic testing to improve early detection. Immunotherapy and personalized medicine approaches are also showing promise, offering hope for more effective treatments in the future.
Coping and Support for Patients
A pancreatic cancer diagnosis can be overwhelming, but patients do not have to face it alone. Support groups, counseling, and patient advocacy organizations provide emotional, financial, and practical assistance. Building a strong support system with family, friends, and healthcare professionals is crucial for coping with the disease.
Conclusion
Understanding how pancreatic cancer is diagnosed is essential for patients, families, and caregivers. Since early detection is key, being aware of the symptoms and risk factors can make a significant difference in survival outcomes.
While pancreatic cancer remains a serious condition, ongoing research, advanced diagnostic methods, and evolving treatment options offer hope. By combining medical care with lifestyle improvements and strong support networks, patients can face the journey with resilience and determination.