When discussing some of the most aggressive forms of cancer, pancreatic cancer consistently appears at the top of the list. Many patients and families often ask: why is pancreatic cancer so deadly? The answer lies in a combination of biological, medical, and lifestyle factors that make this disease one of the most difficult to diagnose and treat effectively.
Pancreatic cancer often develops silently, with minimal symptoms until the disease has progressed to an advanced stage. This late detection, along with the aggressive nature of pancreatic tumor cells, contributes to its high mortality rate. Understanding the disease in detail can help patients, caregivers, and researchers work together toward earlier detection, improved treatments, and better support systems.
Definition and Overview
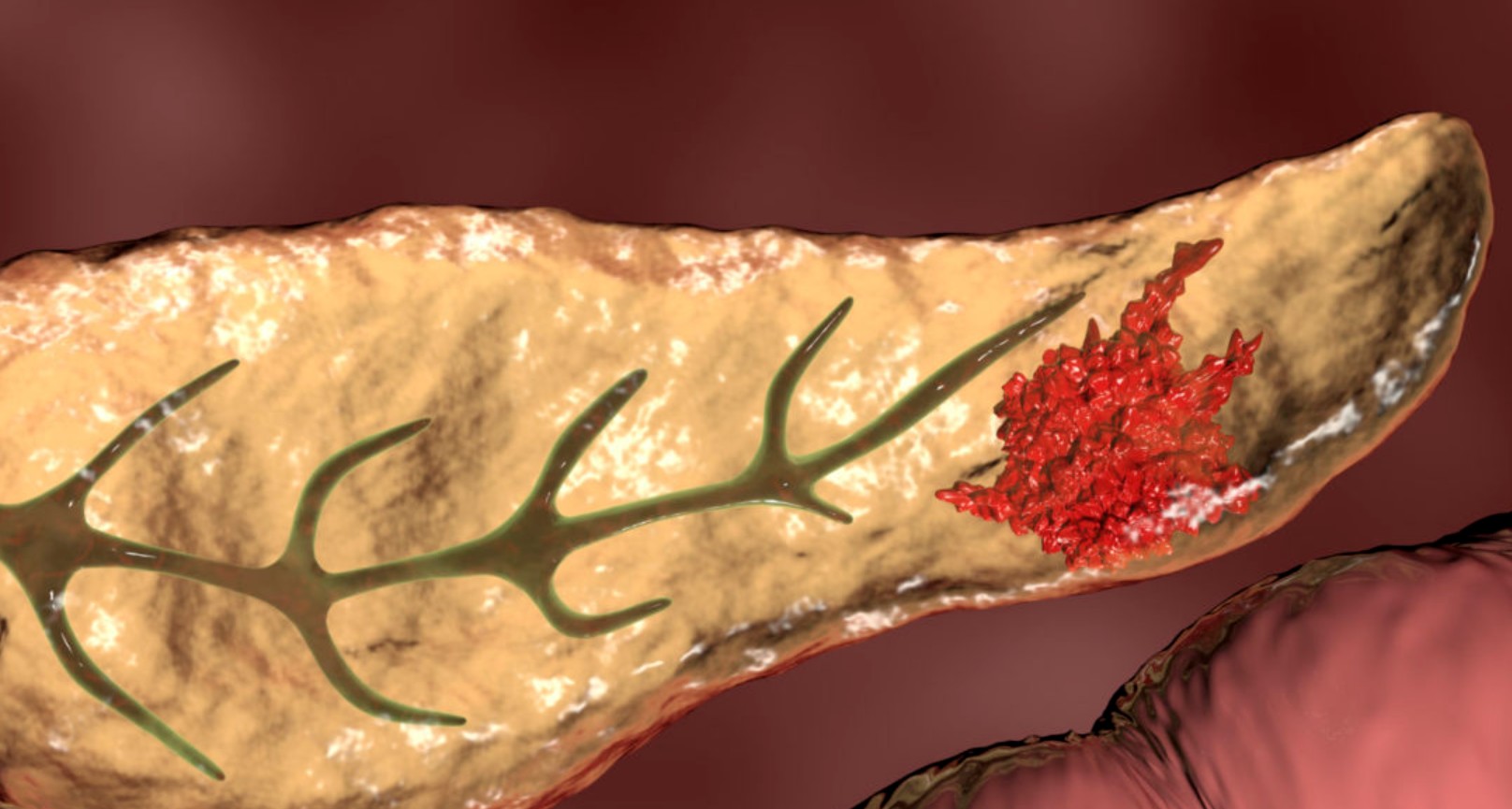
Pancreatic cancer begins in the tissues of the pancreas, an organ located behind the stomach that plays a crucial role in digestion and blood sugar regulation. The most common type is pancreatic ductal adenocarcinoma, which develops in the ducts that carry digestive enzymes. Because the pancreas is deep within the abdomen, tumors are often hidden until they are large or have spread to other organs.
Types of Pancreatic Cancer
There are two main categories of pancreatic cancer:
- Exocrine tumors: These are the most common and include pancreatic adenocarcinoma.
- Endocrine tumors (neuroendocrine tumors or islet cell tumors): Less common, these affect hormone-producing cells of the pancreas.
Each type has different characteristics, progression rates, and treatment approaches.
Causes and Risk Factors
The exact cause of pancreatic cancer is still not fully understood, but several risk factors increase the likelihood of developing the disease:
- Family history of pancreatic cancer
- Genetic mutations (e.g., BRCA1 and BRCA2)
- Chronic pancreatitis
- Smoking and heavy alcohol use
- Obesity and poor diet
- Advanced age, with most cases diagnosed after age 60
Symptoms and Early Warning Signs
One of the main reasons why pancreatic cancer is so deadly is its subtle symptoms. Early warning signs are often vague and may include:
- Unexplained weight loss
- Persistent abdominal or back pain
- Jaundice (yellowing of the skin and eyes)
- Loss of appetite
- Fatigue
- Digestive problems
These symptoms are often mistaken for less serious conditions, delaying diagnosis.
Diagnosis
Diagnosing pancreatic cancer requires a combination of tests, such as:
- Imaging tests (CT scan, MRI, endoscopic ultrasound)
- Blood tests, including tumor markers like CA 19-9
- Biopsy for confirmation
Because symptoms usually appear late, most diagnoses occur when the cancer is already advanced, making treatment more challenging.
Treatment Options
Treatment depends on the stage and type of pancreatic cancer. Options include:
- Surgery: Whipple procedure, distal pancreatectomy, or total pancreatectomy
- Radiation therapy: To shrink tumors and relieve symptoms
- Chemotherapy: Often used in combination with other treatments
- Targeted therapy and immunotherapy: Emerging approaches designed to attack cancer cells more precisely
Despite advances, only a small percentage of patients are eligible for surgery, which offers the best chance of long-term survival.
Prevention and Lifestyle Recommendations
While not all cases can be prevented, certain lifestyle changes can reduce the risk:
- Quit smoking and limit alcohol intake
- Maintain a healthy weight and balanced diet
- Manage diabetes and chronic pancreatitis effectively
- Undergo regular checkups if you have a family history of pancreatic cancer
Prognosis and Survival Rates
The survival rate for pancreatic cancer remains low. According to recent data, the five-year survival rate is about 12%. The aggressive spread of the disease and late diagnosis are the primary reasons why pancreatic cancer is so deadly. Early detection significantly improves the chances of survival, highlighting the importance of awareness and research.
Latest Research and Innovations
Scientists are making progress in developing better diagnostic tools and treatments, such as:
- Liquid biopsy tests to detect cancer earlier
- Personalized medicine based on genetic profiling
- New immunotherapy drugs to boost the body’s defense system
- Minimally invasive surgical techniques to improve recovery
These innovations give hope for more effective treatment in the future.
Coping and Support for Patients
A pancreatic cancer diagnosis can be overwhelming. Emotional support, counseling, and patient support groups play an essential role in improving quality of life. Palliative care, pain management, and nutritional support are equally important in helping patients navigate the physical and emotional challenges of the disease.
Conclusion
So, why is pancreatic cancer so deadly? The answer lies in its silent progression, late diagnosis, and aggressive biology. While treatments are improving, survival rates remain low compared to other cancers. Increased awareness, early screening for high-risk individuals, and ongoing research provide a pathway toward better outcomes. For patients and families, knowledge, support, and proactive healthcare are key.
Frequently Asked Questions
1. Why is pancreatic cancer often diagnosed late?
Because it causes few symptoms in its early stages, most patients are diagnosed only when the disease is advanced.
2. Can pancreatic cancer be cured?
A cure is possible if the cancer is detected early and surgically removed, but this applies to a small percentage of patients.
3. Who is at the highest risk of pancreatic cancer?
People with a family history, genetic predispositions, chronic pancreatitis, or unhealthy lifestyle habits are at higher risk.
4. What is the average life expectancy with pancreatic cancer?
Life expectancy depends on the stage at diagnosis, but advanced cases often have a survival time of less than one year.
5. How can I lower my risk of pancreatic cancer?
By avoiding smoking, maintaining a healthy weight, eating a balanced diet, and getting regular medical checkups, especially if you have risk factors.