Pancreatic cancer is one of the most aggressive forms of cancer, often diagnosed at a late stage when it has already spread to nearby organs. Among the most common metastatic sites, the liver plays a significant role due to its close proximity and blood supply from the pancreas. When pancreatic cancer spreads to the liver, it presents new challenges in treatment, management, and overall prognosis.
Understanding the implications of pancreatic cancer spread to liver can help patients and caregivers make informed decisions. This article explores its definition, symptoms, diagnosis, treatment options, and what patients can expect in terms of survival rates and quality of life.
Definition and Overview
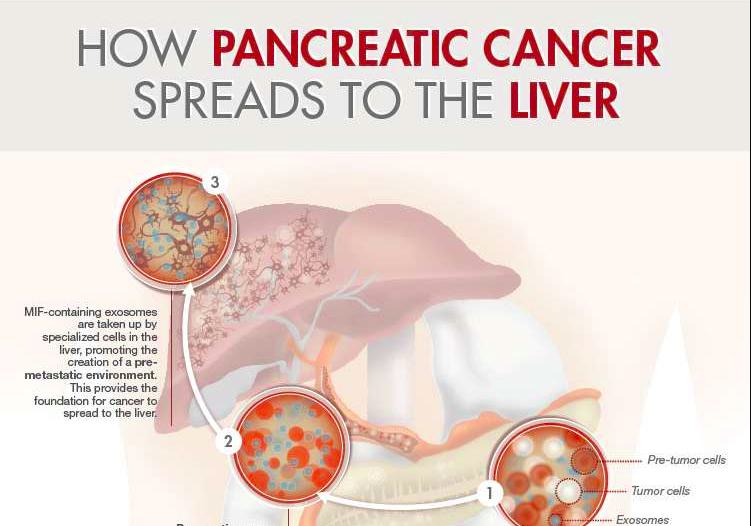
Pancreatic cancer that spreads to the liver is considered stage IV or advanced pancreatic cancer. This happens when cancer cells break away from the pancreas and travel through the bloodstream or lymphatic system to form secondary tumors in the liver. At this stage, the disease is usually not curable, but treatments are available to slow progression, manage symptoms, and improve quality of life.
Types
Pancreatic cancer spread to liver usually originates from two main types of pancreatic cancer:
- Exocrine pancreatic cancer: The most common type, usually adenocarcinoma, which often metastasizes to the liver.
- Neuroendocrine tumors: Less common, may grow more slowly, but can still spread to the liver.
Causes and Risk Factors
Several risk factors increase the likelihood of pancreatic cancer and its spread to the liver, including:
- Genetic mutations such as BRCA1, BRCA2, or KRAS
- Family history of pancreatic or related cancers
- Smoking and excessive alcohol consumption
- Chronic pancreatitis
- Obesity and diabetes
- Older age (most cases occur after age 60)
Symptoms and Early Warning Signs
When pancreatic cancer spreads to the liver, symptoms may become more pronounced, such as:
- Persistent abdominal or back pain
- Unexplained weight loss
- Jaundice (yellowing of skin and eyes)
- Loss of appetite and fatigue
- Swelling in the abdomen due to fluid buildup (ascites)
- Dark urine or pale stools
Because these symptoms often overlap with other conditions, liver metastasis is usually discovered during diagnostic testing.
Diagnosis
Diagnosis of pancreatic cancer spread to liver involves several steps:
- Imaging tests: CT scans, MRI, and PET scans to detect liver lesions.
- Blood tests: Liver function tests and tumor markers like CA 19-9.
- Biopsy: To confirm that tumors in the liver originated from pancreatic cancer.
- Ultrasound: Sometimes used for guided biopsy procedures.
Treatment Options
While pancreatic cancer spread to liver is not usually curable, treatments aim to control growth and relieve symptoms:
- Chemotherapy: Common regimens include FOLFIRINOX or gemcitabine with nab-paclitaxel.
- Targeted therapy: For patients with specific genetic mutations.
- Immunotherapy: Emerging as an option for certain cases.
- Radiation therapy: May be used to reduce pain or control local tumor growth.
- Palliative care: Focused on improving comfort and managing symptoms.
Prevention and Lifestyle Recommendations
Although not all cases are preventable, adopting healthier lifestyle choices may lower risk:
- Avoid smoking and limit alcohol intake
- Maintain a healthy weight and balanced diet
- Stay physically active
- Manage diabetes and other chronic conditions effectively
- Undergo regular check-ups if you have a family history of pancreatic cancer
Prognosis and Survival Rates
Pancreatic cancer spread to liver generally has a poor prognosis due to its aggressive nature. The median survival rate for stage IV pancreatic cancer is typically around 3 to 6 months, but some patients may live longer with treatment. Five-year survival rates remain below 5%. However, new therapies and clinical trials are giving hope for extended survival and improved quality of life.
Latest Research and Innovations
Recent advancements in research are exploring more effective therapies:
- Personalized medicine based on genetic profiling
- New chemotherapy combinations with better outcomes
- Immunotherapy clinical trials targeting tumor-specific markers
- Minimally invasive surgical approaches for symptom relief
These innovations aim to provide better disease control and longer survival for patients with pancreatic cancer that has spread to the liver.
Coping and Support for Patients
Coping with pancreatic cancer spread to liver requires both medical and emotional support. Patients benefit from:
- Counseling and support groups
- Nutritional support to manage weight loss
- Palliative care teams for pain management
- Family and caregiver involvement in daily care decisions
Conclusion
Pancreatic cancer spread to liver represents a serious and advanced stage of the disease. While curative treatment may not be possible, advancements in therapy and supportive care can improve quality of life. Patients and families should discuss options with their healthcare team to make informed decisions and access available resources for support.
FAQ
1. What does it mean when pancreatic cancer spreads to the liver?
It means the cancer has reached stage IV, where cancer cells from the pancreas have traveled to the liver and formed secondary tumors.
2. Can pancreatic cancer with liver metastasis be cured?
Currently, there is no cure, but treatments can help control progression and relieve symptoms.
3. What are common symptoms when pancreatic cancer spreads to the liver?
Symptoms include jaundice, abdominal pain, weight loss, fatigue, and swelling in the abdomen.
4. How long can a patient live with pancreatic cancer spread to the liver?
Survival rates vary, but the average is around 3 to 6 months after diagnosis, depending on treatment and overall health.
5. Are there new treatments for pancreatic cancer spread to liver?
Yes, research is ongoing in targeted therapy, immunotherapy, and advanced chemotherapy options that may extend survival.