Stagescancer.net – Stage 4 pancreatic cancer is a critical and aggressive form of cancer that requires immediate medical attention. It is a life-threatening condition that can be challenging to treat. The pancreas plays a vital role in the body, producing enzymes that aid in digestion and hormones that regulate blood sugar levels.
In this article, we will discuss the life expectancy of patients diagnosed with stage 4 pancreatic cancer. According to the American Cancer Society, the five-year survival rate for stage 4 pancreatic cancer is only 3%. However, it is essential to note that every individual’s case is unique and can vary depending on various factors.
We will explore the prognosis and various factors that can affect life expectancy. Additionally, we will discuss the available treatment options, including palliative care methods and clinical trials. We understand that it can be a challenging journey, and we will also provide guidance on emotional well-being and coping strategies. Lastly, we will emphasize the importance of seeking professional guidance and support throughout the journey.
If you or a loved one has been diagnosed with stage 4 pancreatic cancer, this article seeks to inform you on the best approaches to navigate this difficult time.
What is Stage 4 Pancreatic Cancer?
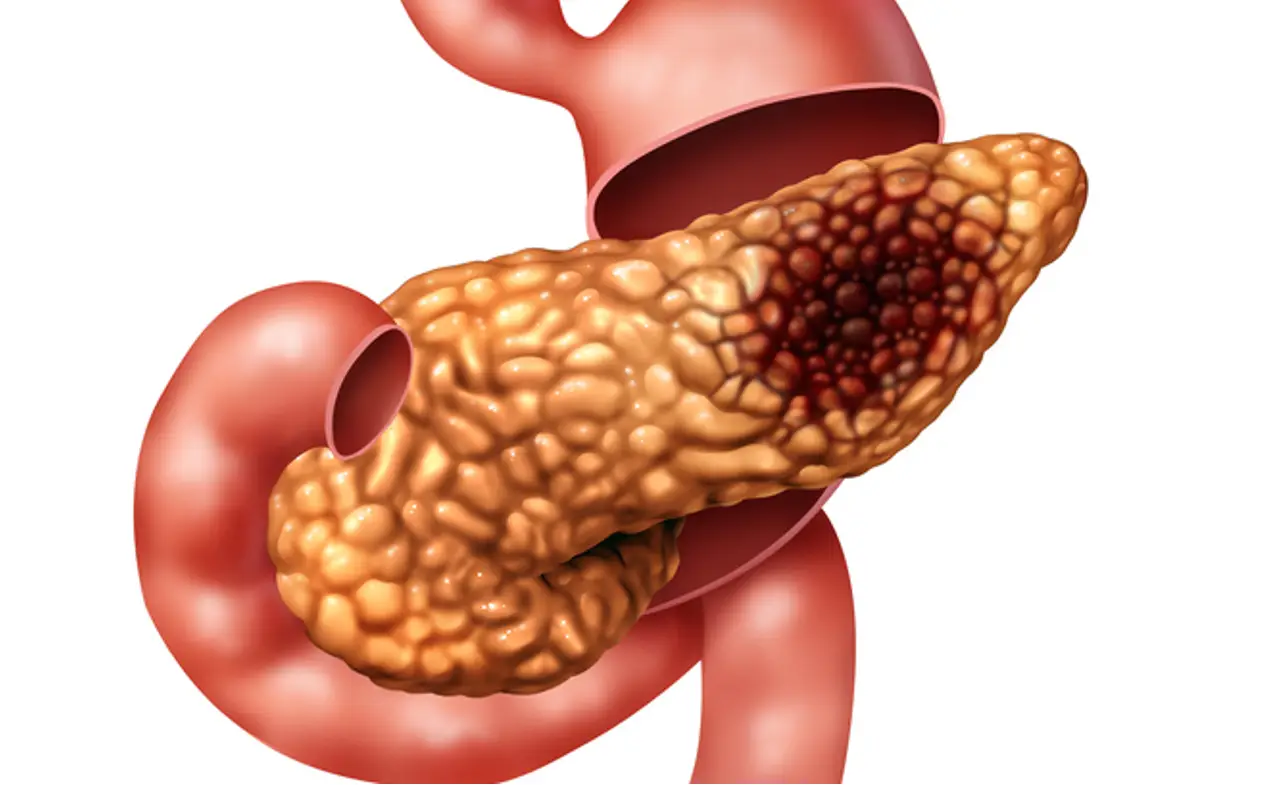
Pancreatic cancer is a type of cancer that forms in the tissues of the pancreas. Stage 4 pancreatic cancer is an advanced stage of the disease. At this stage, cancer has spread to other organs, making it more challenging to treat.
Unlike earlier stages of pancreatic cancer, stage 4 pancreatic cancer is accompanied by more severe symptoms and complications. These may include pain, jaundice, weight loss, or blood clots.
Stage 4 pancreatic cancer is typically diagnosed using a combination of imaging tests such as CT scan, MRI, or PET scan and biopsies. Once diagnosed, treatment for stage 4 pancreatic cancer aims to control symptoms, improve the quality of life, and prolong survival as much as possible.
Palliative care and supportive measures play a critical role in managing symptoms and helping patients cope with the impact of the disease. Various treatment options are available, including surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy.
If you or a loved one has been diagnosed with stage 4 pancreatic cancer, it is essential to seek professional guidance and support throughout the journey. With a full understanding of the disease and available treatment options, it is possible to improve the quality of life and prolong survival.
Factors Affecting Life Expectancy
The life expectancy of individuals with stage 4 pancreatic cancer can be influenced by multiple factors. Both patient-specific factors and disease-related factors play a role in determining the prognosis and survival rates for this advanced stage.
Patient-Specific Factors
Various patient-specific factors can impact the outcome of stage 4 pancreatic cancer. These include:
- Age: Older patients generally have a lower life expectancy than younger patients.
- Overall Health: Patients with additional health conditions may have decreased survival rates.
- Response to Treatment: Patients who respond well to treatment typically have better outcomes.
- Emotional Support: Patients who have a strong support system may have better mental and emotional well-being, which can positively impact their overall health.
Disease-Related Factors
In addition to patient-specific factors, certain disease-related factors can contribute to the life expectancy of individuals with stage 4 pancreatic cancer. These include:
| Factor | Description |
|---|---|
| Tumor size | Larger tumors may be more difficult to treat and may indicate a more advanced stage of the disease. |
| Cancer Spread | The location and extent of cancer spread can impact the prognosis and treatment options available. |
| Cancer Type | The specific type of pancreatic cancer can impact the disease progression and response to treatment. |
| Overall Health | A patient’s overall health can also affect the prognosis and life expectancy of individuals with stage 4 pancreatic cancer. |
Understanding these factors can help patients and their healthcare team make informed decisions about treatment and care. While some factors may be beyond an individual’s control, others can be managed with proper support and treatment approaches.
Average Life Expectancy for Stage 4 Pancreatic Cancer
Stage 4 pancreatic cancer is an advanced stage of the disease that comes with a poor prognosis. On average, patients diagnosed with this stage have a life expectancy range of approximately three to six months (American Cancer Society).
However, it’s important to note that this figure is an average and there are individual variables that can greatly influence life expectancy. Factors such as a patient’s overall health, age, and response to treatment can all play a role in determining survival rates.
Additionally, treatment options are available and can extend a patient’s life. Some individuals with stage 4 pancreatic cancer have surpassed the average life expectancy range, and with advancements in cancer research and development of novel treatments, there is hope for improved survival rates in the future.
It’s important for patients to speak with their healthcare providers to discuss and develop a personalized treatment plan tailored to their specific needs and circumstances. Having a supportive network of family, friends, and healthcare professionals can also provide emotional support and guidance throughout the cancer journey.
Treatment Options for Stage 4 Pancreatic Cancer
Patients diagnosed with stage 4 pancreatic cancer have limited treatment options, and determining the appropriate course of action can be complex. Treatment plans typically involve a multifaceted approach that may include:
- Surgery: Depending on the patient’s health, location of the tumor, and other factors, surgical removal of the tumor may be an option. However, surgery is generally not recommended for stage 4 pancreatic cancer.
- Chemotherapy: This treatment involves the use of drugs to kill cancer cells throughout the body. It’s often the primary treatment for stage 4 pancreatic cancer, either as a standalone treatment or in combination with other approaches.
- Radiation Therapy: Radiation therapy uses high-energy radiation to destroy cancer cells. It is usually administered alongside chemotherapy, and may help shrink the tumor.
- Targeted Therapy: This type of treatment targets specific genes or proteins that contribute to the growth and spread of cancer. It can be used as an alternative or in combination with chemotherapy.
- Immunotherapy: Immunotherapy is a type of treatment that harnesses the body’s immune system to fight cancer. It’s a relatively new approach for pancreatic cancer and is still largely experimental.
The efficacy of these treatments can vary depending on the patient’s age, overall health, and other factors. Your healthcare team will help determine which combination of treatments is best for your case.
Palliative Care and Supportive Measures
For individuals with stage 4 pancreatic cancer, palliative care and supportive measures are crucial in helping to manage symptoms and improve quality of life. Palliative care is specialized medical care that focuses on providing relief from pain, stress, and other symptoms of serious illness.
Pain management is an important aspect of palliative care for those with stage 4 pancreatic cancer. Pain can be caused by tumors pressing on organs or nerves, or by chemotherapy or radiation therapy. Medications, physical therapy, and nerve blocks are common methods of pain management.
Nutritional support is also a key component of palliative care for individuals with stage 4 pancreatic cancer. The disease can impact a person’s ability to eat and digest food, leading to malnutrition and weight loss. A registered dietitian can help develop an individualized nutrition plan and recommend supplements or tube feeding if necessary.
Emotional support is equally important as physical support in palliative care for individuals with stage 4 pancreatic cancer. The diagnosis of this advanced stage can be overwhelming and it can cause anxiety, depression, and other psychological symptoms. Counseling, support groups, and family therapy can help manage these emotional concerns.
Supportive measures can also be taken to improve quality of life for individuals with stage 4 pancreatic cancer. This can include home health care, hospice care, and other services that enable patients to remain in their homes and receive necessary care. It’s important to discuss these options with healthcare providers and loved ones early in the care process to ensure the best possible outcome.
Clinical Trials and Experimental Treatments
Experimental treatments and clinical trials are an important option for patients with stage 4 pancreatic cancer. These treatments allow patients to access innovative therapies that aren’t available through standard care. Clinical trials are carefully designed studies that evaluate the effectiveness and safety of new interventions and procedures. There are several types of clinical trials, and patients often participate in phase I or phase II trials that test new drugs or combinations of treatments.
While participating in clinical trials comes with some risks, including potential side effects and uncertainties about the effectiveness of the treatment, it can also offer significant benefits. Patients in clinical trials often receive more careful monitoring and follow-up care, as well as access to cutting-edge treatments before they are available to the general public.
The Significance of Clinical Trials for Stage 4 Pancreatic Cancer
Clinical trials are particularly significant for patients with stage 4 pancreatic cancer because there are limited treatment options available. Patients who have exhausted traditional therapies may benefit from experimental treatments that could slow the progression of their disease or even eliminate the cancer altogether.
How to Find Clinical Trials
Patient advocacy organizations and medical institutions can provide information about clinical trials and how to enroll. Patients can also search online databases that list current trials, such as the National Institutes of Health’s ClinicalTrials.gov website.
Experimental Treatments
Besides clinical trials, experimental treatments can also be an option for stage 4 pancreatic cancer patients. These treatments include drugs that are still in development or that have been approved but are used in a different way from the standard approach. Patients who are interested in pursuing experimental treatments should discuss this option with their healthcare provider to determine if it’s safe and appropriate for their situation.
Coping Strategies and Emotional Well-being
Being diagnosed with stage 4 pancreatic cancer can be a daunting experience, and it’s normal to feel a range of emotions, from fear to sadness and anger. Coping with the diagnosis and treatment can impact emotional well-being, and it’s essential to recognize the importance of maintaining mental health throughout the process.
One effective coping strategy is seeking support from loved ones, friends, and support groups. Talking about your feelings and concerns can help ease anxiety and provide a sense of comfort through challenging times. Additionally, some patients find comfort in meditation, yoga, or other relaxation techniques that promote stress-relief.
It’s also crucial to take care of physical health by eating a healthy diet, exercising, and getting enough sleep. Keeping a healthy routine can help improve emotional well-being and alleviate symptoms.
Finally, it’s vital to recognize when to seek professional guidance and support. Mental health professionals, such as psychologists and therapists, can provide invaluable insight and guidance to help maintain emotional well-being throughout the journey.
Hope and Positivity for Stage 4 Pancreatic Cancer
When facing a diagnosis of stage 4 pancreatic cancer, it can feel overwhelming and isolating. However, it’s important to know that you are not alone. There is hope and positivity to be found, even in the midst of difficult times.
Survivor stories are an excellent source of inspiration and encouragement. Many people have beaten the odds and are thriving years after their stage 4 pancreatic cancer diagnosis. These stories can provide a sense of hope and possibility, reminding us that even the most dire circumstances can be overcome.
Uplifting messages and quotes can also offer a boost of positivity. Whether it’s a favorite saying, a mantra, or a reminder of life’s simple pleasures, finding and holding onto a positive message can help shift your mindset and bring a sense of calm and purpose.
Finally, building a support system of friends, family, and healthcare professionals can make all the difference. Surrounding yourself with positive influences and individuals who lift you up can provide a sense of community and emotional support throughout your journey.
Seeking Professional Guidance and Support
Receiving a diagnosis of stage 4 pancreatic cancer can be overwhelming, and it is essential to seek professional guidance and support. This can include healthcare providers, support groups, and organizations that specialize in pancreatic cancer care.
Expert medical professionals, including oncologists and palliative care teams, can offer valuable assistance and information on treatment options, managing symptoms, and improving quality of life. They can also connect patients and their families with additional resources, such as social workers, financial counselors, and nutritionists.
In addition, support groups and organizations can provide emotional support and practical resources for those affected by stage 4 pancreatic cancer. They can offer a sense of community and shared experiences, as well as educational materials and advocacy efforts.
Remember, seeking professional guidance and support is not a sign of weakness. It is a crucial step in the journey towards managing stage 4 pancreatic cancer and ensuring the best possible outcomes for you and your loved ones.
FAQ
What is the life expectancy for stage 4 pancreatic cancer?
The life expectancy for stage 4 pancreatic cancer varies depending on various factors such as the individual’s overall health, treatment options, and response to treatment. On average, the survival rate for stage 4 pancreatic cancer is relatively low, with a five-year survival rate of around 1%. It is essential to consult with a healthcare professional for a personalized prognosis and treatment plan.
What are the treatment options for stage 4 pancreatic cancer?
Treatment options for stage 4 pancreatic cancer may include surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy. The specific treatment plan will depend on the individual’s overall health, tumor characteristics, and other factors. It is crucial to consult with a healthcare team to determine the most suitable treatment approach.
What factors can affect the life expectancy of individuals with stage 4 pancreatic cancer?
Several factors can influence the life expectancy of individuals with stage 4 pancreatic cancer. These factors include the extent of tumor spread, response to treatment, overall health and fitness, age, and the presence of other medical conditions. It is important to remember that each individual’s situation is unique, and a healthcare professional can provide personalized insights.
What is palliative care, and how does it benefit individuals with stage 4 pancreatic cancer?
Palliative care focuses on improving the quality of life of individuals with serious illnesses, including stage 4 pancreatic cancer. It includes pain management, symptom control, psychological and emotional support, and assistance with practical aspects of daily life. Palliative care aims to maximize comfort and well-being for both the patient and their loved ones.
Are there clinical trials or experimental treatments available for stage 4 pancreatic cancer?
Yes, there are ongoing clinical trials and experimental treatments for stage 4 pancreatic cancer. Clinical trials offer the opportunity to access innovative therapies and contribute to medical research. However, participation in clinical trials should be discussed with a healthcare team to determine eligibility, potential risks, and benefits.
What resources are available for emotional support for individuals with stage 4 pancreatic cancer?
Emotional support is essential for individuals with stage 4 pancreatic cancer, and there are several resources available. Support groups, therapy, counseling services, and online communities can provide a space to share experiences, express emotions, and receive guidance from others who understand the challenges of living with the disease. Healthcare providers can also refer patients to reputable organizations that offer emotional support specific to pancreatic cancer.
Where can individuals with stage 4 pancreatic cancer find professional guidance and support?
Individuals with stage 4 pancreatic cancer can seek professional guidance and support from various sources. Specialized oncology centers, pancreatic cancer treatment facilities, and healthcare professionals experienced in managing pancreatic cancer can offer valuable guidance and personalized treatment plans. Additionally, organizations such as the American Cancer Society and Pancreatic Cancer Action Network provide resources, education, and support for individuals and their families.