Stagescancer.net – Pancreatic cancer can have a significant impact on a person’s health, and the development of ascites can further complicate the situation. Ascites is the buildup of fluid in the abdominal cavity, which can cause discomfort and other symptoms. In pancreatic cancer patients, ascites is often an indicator of advanced disease, and understanding its impact on life expectancy is crucial for managing the condition.
In this article, we will delve into the basics of pancreatic cancer and ascites, explore the connection between ascites and life expectancy, and discuss the various factors that can influence life expectancy for those living with pancreatic cancer and ascites. We will also provide insights into treatment options, coping strategies, and supportive resources available to patients and their caregivers.
By empowering patients with knowledge and support, we hope to improve the quality of life for those who are facing pancreatic cancer ascites and help them navigate this difficult journey with greater confidence.
Understanding Pancreatic Cancer and Ascites
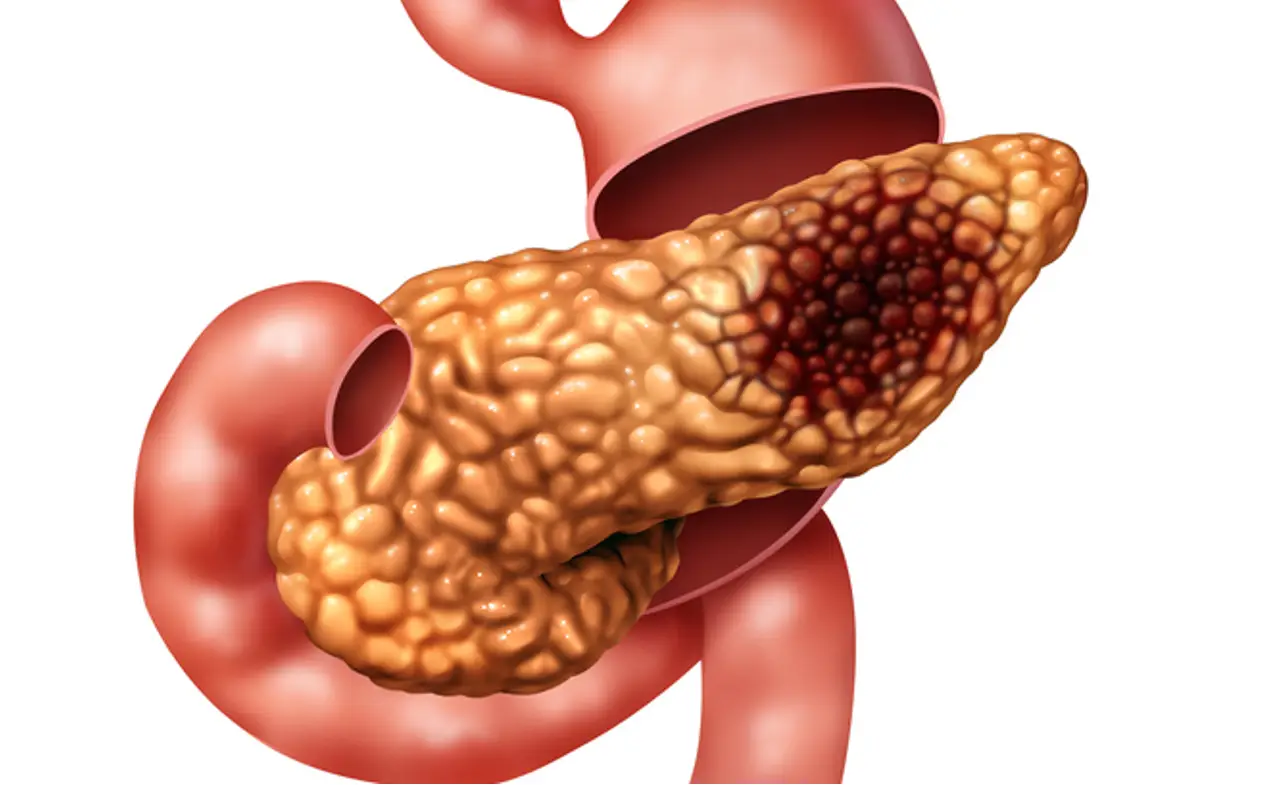
Pancreatic cancer is a type of cancer that starts in the pancreas, the gland that sits behind the stomach. Symptoms of pancreatic cancer may include jaundice, abdominal pain, weight loss, and digestive problems. Risk factors for pancreatic cancer include smoking, obesity, diabetes, and family history.
Ascites is a condition where fluid accumulates in the abdomen, causing swelling and discomfort. In pancreatic cancer patients, ascites can develop due to the tumor blocking the lymphatic system or the liver, causing excess fluid buildup. Ascites can negatively impact overall health by putting pressure on organs, causing difficulty breathing, and increasing the risk of infection.
Understanding the basics of pancreatic cancer and ascites is essential in managing this condition. If you or a loved one has been diagnosed with pancreatic cancer and ascites, seeking appropriate medical care and support can make a significant difference in quality of life and life expectancy.
The Connection Between Ascites and Life Expectancy
Ascites, the buildup of fluid in the abdomen, commonly occurs in patients with pancreatic cancer and can significantly impact their overall health and life expectancy. The presence of ascites can lead to increased complications and a reduced ability to tolerate treatment, making it essential for healthcare professionals to assess and monitor its impact regularly.
When discussing life expectancy, it’s crucial to consider the presence of ascites as a key factor. The extent and progression of ascites in pancreatic cancer patients can affect the efficacy of treatments and the potential for disease progression. Therefore, early detection and treatment of ascites are vital in improving outcomes and enhancing patient survival rates.
Healthcare professionals should work collaboratively with patients to tailor treatment plans that incorporate interventions for managing ascites and addressing related symptoms. Regular imaging and fluid drainage procedures may help address ascites-related concerns and improve patients’ overall quality of life. Effective communication and supportive care for both patients and their caregivers are essential in managing pancreatic cancer with ascites.
Factors Influencing Life Expectancy in Pancreatic Cancer Ascites
There are several factors that can influence the life expectancy of individuals with pancreatic cancer and ascites. These factors include:
| Factors | Description |
|---|---|
| Stage of cancer | Pancreatic cancer is often diagnosed in the later stages, which can have a significant impact on life expectancy. The earlier the cancer is detected, the higher the chances of successful treatment. |
| Extent of ascites | The amount of ascites present in the body can also impact life expectancy. Large amounts of ascites can cause discomfort and complications that can affect overall health. |
| Overall Health | The overall health of the individual, including age and other pre-existing medical conditions, can also impact life expectancy. Individuals in good health may have a better chance of responding well to treatment and managing the condition long-term. |
| Treatment options | The type and effectiveness of treatment options available will also play a role in estimating life expectancy. Depending on the stage and progression of the cancer, treatment options can vary. |
It is important to consider these factors when estimating life expectancy to provide individuals and their healthcare teams with accurate information and appropriate treatment plans. However, it is important to note that each case is unique, and individual circumstances will also impact life expectancy.
Prognosis and Survival Rates for Pancreatic Cancer Ascites
When it comes to pancreatic cancer with ascites, the prognosis can vary widely depending on several factors. These may include the stage and subtype of pancreatic cancer, the extent and severity of ascites, and the overall health of the patient.
While it can be challenging to predict life expectancy with precision, it is essential to seek personalized assessments and discuss prognosis with healthcare professionals. Doing so can provide a clearer understanding of the individual’s condition and assist in making informed decisions about treatment options and other major life decisions.
According to the American Cancer Society, the five-year survival rate for pancreatic cancer with ascites is around 3%. However, these rates can vary widely depending on the specific subtype and stage of the disease. For example, the five-year survival rate for localized pancreatic cancer without ascites is around 39%, while for metastatic pancreatic cancer, it drops to 3%.
| Subtype of Pancreatic Cancer | Stage | Five-Year Survival Rate |
|---|---|---|
| Adenocarcinoma | Localized | 39% |
| Adenocarcinoma | Regional | 12% |
| Adenocarcinoma | Metastatic | 3% |
| Neuroendocrine Tumor | Localized | 61% |
| Neuroendocrine Tumor | Regional | 52% |
| Neuroendocrine Tumor | Metastatic | 15% |
It’s important to note that statistics may not reflect an individual’s unique experience, and there are factors that can influence survival rates. These can include the effectiveness of treatment, the individual’s response to treatment, and access to follow-up care.
In conclusion, while prognosis and survival rates are important factors to consider in pancreatic cancer with ascites, there is hope. Advances in research and treatment approaches, along with emotional and psychological support, can help empower patients and improve the quality of life. It’s essential to stay informed, seek support, and communicate openly with healthcare professionals to make the best decisions for individual care and needs.
Treatment Options for Pancreatic Cancer Ascites
When it comes to managing pancreatic cancer ascites, there are various treatment options available. The choice of treatment depends on factors such as the type and stage of cancer, extent of ascites, overall health, and personal preferences.
Medical Interventions
Chemotherapy: This treatment involves the use of medications to kill cancer cells. It’s often used in combination with other treatments for pancreatic cancer and may be administered orally or through an intravenous (IV) injection.
Radiation Therapy: This treatment uses high-energy radiation to destroy cancer cells. It may be delivered externally or internally and can be used in combination with chemotherapy or targeted therapy.
Targeted Therapy: This treatment involves the use of medications that target specific genes, proteins, and other molecules involved in the growth and spread of cancer cells. It’s often used when the cancer has spread to other parts of the body.
Non-Medical Interventions
Palliative Care: This treatment is focused on relieving symptoms, reducing pain, and improving the quality of life for individuals with pancreatic cancer and ascites. It can involve a team of healthcare professionals, including a palliative care specialist, who provide emotional, physical, and spiritual support.
Multidisciplinary Approach: This treatment involves the collaboration of various healthcare professionals, including oncologists, surgeons, radiologists, pain specialists, and nutritionists. They work together to provide a comprehensive treatment plan that is tailored to meet the specific needs of the patient.
Personalized Treatment Plans
Since every individual is unique, personalized treatment plans can improve the quality of care and outcome. The treatment plan should be based on specific personal circumstances and calculated risks, ensuring that patients get the best possible care.
It is essential to speak with a healthcare professional to determine the best treatment options for pancreatic cancer ascites and its wider health impacts.
Palliative Care and End-of-Life Considerations
For individuals with pancreatic cancer and ascites, palliative care and end-of-life considerations play a crucial role in improving quality of life. Palliative care is a specialized medical care approach that focuses on symptom management, pain relief, and emotional support, rather than curative treatment. It can be especially helpful for those with advanced-stage pancreatic cancer and ascites, for whom cure is not possible.
Palliative care aims to provide relief from symptoms like pain, nausea, and fatigue that can impact overall well-being. It involves a multidisciplinary approach that includes healthcare providers like nurses, doctors, and social workers who work together to address patient needs. This approach can also help manage emotional and psychological distress, such as anxiety, depression or grief.
| Type of Symptom Relief | Possible Forms of Palliative Care |
|---|---|
| Physical symptoms like pain | Medications, Physiotherapy |
| Emotional or psychological distress | Counseling, Psychotherapy, Mindfulness Meditation |
| Spiritual Distress or Existential Crisis | Chaplaincy, Spiritual Exploration, Support Groups |
End-of-life care planning is a natural extension of palliative care. It aims to ensure that the patient’s wishes and values are respected and addressed in the dying phase. The decision to consider end-of-life care is deeply personal and may involve discussions with family members and caregivers. As sickness progresses, patients may become unable to make decisions for themselves. Therefore, advanced care planning includes appointing a proxy to make the decisions the patients can’t.
For those with pancreatic cancer and ascites, hospice care can be a viable option. This form of care allows one to live in peace, maintain dignity, and avoid unhelpful treatments. Hospice care provides pain relief, limited treatments, and spiritual and emotional support. This help aids the patient in managing the end of life journey.
Palliative care and end-of-life considerations provide crucial support for individuals with pancreatic cancer and ascites. By optimizing symptom management and addressing emotional and spiritual needs, these approaches can help improve overall quality of life, even in challenging circumstances.
Coping Strategies and Support for Patients and Caregivers
Dealing with pancreatic cancer ascites can be challenging and complex, both physically and emotionally, for both patients and caregivers. There are many coping strategies and support resources available to help navigate these difficulties.
Firstly, it is important to acknowledge and express your feelings. It is alright to experience a range of emotions, such as fear, anger, and sadness. Talking to friends, family, or a mental health professional can be helpful in dealing with these emotions.
Self-care practices, such as exercise, healthy eating, and relaxation techniques, can also help improve physical and emotional well-being. It is important to get enough rest and manage stress as much as possible.
Joining a support group can bring a sense of community and understanding. Support groups allow individuals to connect with others going through similar experiences, which can help provide emotional support and practical advice.
Professional counseling can also help individuals learn coping strategies and problem-solving skills. Social workers or therapists can offer assistance with financial, legal, or other practical issues.
Remember that seeking support is a sign of strength, and there is no shame in asking for help. There are many resources available for both patients and caregivers to manage the challenges associated with pancreatic cancer ascites.
Advances in Research and Promising Therapies
Despite the challenges of treating pancreatic cancer with ascites, ongoing advances in research and promising therapies provide hope for patients and their families. Clinical trials are exploring new treatment options, including innovative drug combinations that target cancer cells while minimizing harm to healthy tissue.
One promising area of research focuses on immunotherapy, which aims to boost the immune system’s ability to recognize and attack cancer cells. Another promising treatment is called HIPEC (hyperthermic intraperitoneal chemotherapy), a surgical procedure that delivers heated chemotherapy directly to the abdomen.
Additionally, researchers continue to explore ways to improve diagnostic methods and detect pancreatic cancer at earlier stages, when treatment is most effective. As more is learned about the genetics and molecular makeup of pancreatic cancer cells, it is hoped that personalized treatment plans will become more effective in managing the disease.
While there is still much to learn about pancreatic cancer with ascites, ongoing research provides hope for a better future.
Lifestyle Measures to Improve Overall Well-being
Individuals with pancreatic cancer and ascites can benefit from incorporating lifestyle measures into their treatment plan to support overall health. Adopting a multifaceted approach to well-being can help manage symptoms, improve quality of life, and enhance resilience.
1. Balance Diet
Eating a balanced diet with plenty of fruits, vegetables, complex carbohydrates, and lean protein can help support the immune system, lower inflammation and maintain healthy body weight. Those with pancreatic cancer ascites should consult with their healthcare team to ensure their diet aligns with their specific nutritional needs.
2. Regular Exercise
Regular exercise under the guidance of a healthcare professional can improve strength, stamina, and overall fitness. It can also help stimulate appetite, reduce fatigue, and improve mood.
3. Stress Management Techniques
Effective management of stress can improve emotional well-being and may also improve physical symptoms. Stress management techniques such as meditation, deep breathing exercises, and mindfulness practices can be helpful.
4. Complementary Therapies
Complementary therapies such as acupuncture, massage therapy, and yoga can help manage symptoms related to pancreatic cancer ascites. However, it is essential to discuss such therapies with healthcare professionals first.
Overall, adapting to a healthy lifestyle can help individuals with pancreatic cancer ascites improve overall health and well-being. It is crucial to consult with healthcare professionals before implementing any lifestyle changes.
Communication with Healthcare Professionals
Effective communication with healthcare professionals is crucial for individuals with pancreatic cancer and ascites. It helps to ensure that patients receive optimal care and support tailored to their unique needs and circumstances. It is essential to build a collaborative and supportive relationship with the healthcare team, consisting of oncologists, nurses, social workers, and others.
Patient and caregiver involvement is essential in the decision-making process to ensure that the care aligns with their goals, preferences, and values. It’s essential to speak up and ask any questions or share concerns. Patients should provide their healthcare team with accurate and honest information about their symptoms, mood, and treatment side effects as well.
How to communicate effectively with healthcare professionals?
Effective communication with healthcare professionals can enhance the quality of life of patients with pancreatic cancer and ascites. Here are some tips on how to facilitate open and effective communication:
- Prepare a list of questions and concerns before each appointment
- Keep a notebook to record information and notes
- Use simple language and avoid technical jargon
- Be honest and accurate when reporting symptoms and side effects
- Seek clarification if anything is unclear
- Speak up if you have any concerns or questions
- Involve family members or friends if needed
Emotional and Psychological Impact of Pancreatic Cancer Ascites
Pancreatic cancer and ascites can have a significant emotional and psychological impact on patients and their families. The diagnosis of cancer can evoke a range of emotional responses such as anxiety, fear, and uncertainty. Living with ascites, a condition that can cause discomfort and pain, can also contribute to emotional distress.
It is essential to acknowledge and address these emotional responses and seek appropriate support. Patients can benefit from talking to their healthcare providers or a mental health professional about their concerns. They can also explore complementary therapies such as yoga, meditation, or art therapy to help manage stress and improve their mental health.
Caregivers and family members of patients with pancreatic cancer and ascites may also experience emotional strain. Coping strategies such as engaging in support groups and seeking respite care may help alleviate some of this burden.
The emotional and psychological impact of pancreatic cancer and ascites cannot be underestimated. Support and appropriate care can help patients and families better manage these challenges and improve their quality of life.
Patient Stories and Inspiring Journeys
In this section, we feature the stories of real people who have faced pancreatic cancer and ascites. These inspiring journeys offer personal insights into the challenges and triumphs of living with this diagnosis.
Ava’s tenacity in the face of a difficult diagnosis
Ava, a 65-year-old grandmother, was diagnosed with stage IV pancreatic cancer with ascites. Despite the difficult prognosis, Ava remained positive and determined.
“I knew that I had to keep fighting and remain hopeful. I am grateful for the support of my family and doctors, who have helped me maintain my strength and continue to live life as fully as possible,” says Ava.
Through Ava’s journey, we learn about the importance of resilience and hope in navigating this diagnosis.
David’s journey of self-discovery
David, a 50-year-old business executive, was diagnosed with pancreatic cancer with ascites during a routine checkup. While devastated by the news, David used this experience as an opportunity for self-discovery.
“I realized that I had been living my life on autopilot and that I needed to make changes to prioritize my health and well-being,” David shares.
David’s journey highlights the value of self-reflection and personal growth during difficult times.
Lena’s advocacy for improved support
Lena, a 38-year-old mother of two, was diagnosed with advanced pancreatic cancer with ascites. Throughout her treatment journey, Lena noticed a lack of support and resources available for individuals with this diagnosis.
“I became an advocate for improved support and resources for those affected by pancreatic cancer with ascites. I want other patients and their families to have access to the same level of care and compassion that I received,” Lena says.
By sharing her story, Lena raises awareness of the need for improved support systems and encourages others to speak out for change.
These patient stories serve as poignant reminders of the resilience, strength, and hope that are possible in the face of pancreatic cancer with ascites. They inspire us to continue working towards better treatments, improved support, and a brighter future for all those affected by this diagnosis.
Supportive Resources for Pancreatic Cancer Ascites
Dealing with pancreatic cancer and ascites can be challenging, both emotionally and physically. However, there are numerous supportive resources available to assist patients and their caregivers in navigating this difficult journey.
Websites:
- American Cancer Society: The American Cancer Society provides a wealth of information on pancreatic cancer and ascites, including details about diagnosis, treatment, and support services.
- Pancreatic Cancer Action Network: The Pancreatic Cancer Action Network is a nonprofit organization that provides resources and support for patients and their families affected by pancreatic cancer.
- Pancare Foundation: Pancare Foundation is a charity focused on helping pancreatic cancer patients with informational resources, support services, and medical research.
- Cancer Support Community: This website offers forums and support groups for patients and their caregivers to connect with others who understand what they are going through.
Organizations:
- Pancreatic Cancer Action Network: The Pancreatic Cancer Action Network offers a variety of support services, including peer-to-peer support, caregiver resources, and survivor programs.
- American Pancreatic Association: The American Pancreatic Association is a professional organization dedicated to advancing research, treatment, and education related to pancreatic diseases.
- Hope for Pancreatic Cancer: This organization offers a hotline for patients and caregivers seeking information and support related to pancreatic cancer and ascites.
Helplines:
- Call 1-877-272-6226 to speak with a Pancreatic Cancer Action Network patient services representative and obtain information about resources and support options.
- The American Cancer Society’s helpline offers 24/7 assistance to individuals affected by cancer. Call 1-800-227-2345 to speak with a representative.
Support Groups:
- Pancreatic Cancer Action Network: Offers online and in-person support groups for pancreatic cancer patients and their caregivers.
- Patient Support Groups: Many hospitals and cancer centers offer patient support groups focused on pancreatic cancer and ascites.
It is essential to remember that there are supportive resources, and seeking assistance and support can provide valuable emotional and practical support during this difficult journey.
Conclusion: Empowering Patients and Improving Quality of Life
Living with pancreatic cancer and ascites can be challenging, but it’s important to remember that there is always hope. By understanding the condition, seeking appropriate medical care, and maintaining a positive attitude, patients can take an active role in their care and improve their quality of life.
Empowering patients through education, emotional support, and involvement in decision-making is crucial in managing pancreatic cancer with ascites. The importance of palliative care, end-of-life considerations, and support for both patients and caregivers cannot be overstated.
Despite the challenges, advances in research and emerging therapies offer hope for improving life expectancy and quality of life for patients with pancreatic cancer and ascites. By staying informed, advocating for their well-being, and taking steps to maintain overall health, individuals can navigate their pancreatic cancer journey with confidence and resilience.
At the end of the day, pancreatic cancer and ascites can be overwhelming, but patients are not alone. Through supportive resources, community involvement, and a collaborative healthcare team, patients can find the strength and support they need to face the challenges ahead.
Let’s work together to empower patients, improve quality of life, and continue to support those affected by pancreatic cancer with ascites.
FAQ
What is pancreatic cancer ascites?
Pancreatic cancer ascites is the accumulation of fluid in the abdominal cavity, specifically in the peritoneal space, as a result of pancreatic cancer.
How does ascites develop in pancreatic cancer patients?
Ascites may develop in pancreatic cancer patients when cancer cells block the lymphatic system, impairing the drainage of fluid from the abdominal cavity.
What is the impact of ascites on overall health?
Ascites can significantly impact overall health by causing abdominal discomfort, bloating, difficulty breathing, and reduced appetite.
How does ascites affect life expectancy in pancreatic cancer patients?
The presence of ascites in pancreatic cancer patients can negatively affect life expectancy, as it is often associated with more advanced stages of the disease and may limit treatment options.
What factors influence life expectancy in individuals with pancreatic cancer ascites?
Several factors can influence life expectancy in individuals with pancreatic cancer ascites, including the stage of cancer, extent of ascites, overall health, and treatment options.
What is the prognosis for pancreatic cancer with ascites?
The prognosis for pancreatic cancer with ascites depends on various factors, such as the stage and subtype of cancer, overall health, and response to treatment.
What are the treatment options for managing pancreatic cancer ascites?
Treatment options for managing pancreatic cancer ascites may include chemotherapy, radiation therapy, targeted therapy, and palliative care to alleviate symptoms.
How can palliative care and end-of-life considerations improve quality of life?
Palliative care can provide symptom management, pain relief, and emotional support to improve the quality of life for individuals with pancreatic cancer and ascites. End-of-life considerations, such as hospice care and advanced care planning, can also ensure comfort and dignity.
Are there coping strategies and support available for patients and caregivers?
Yes, there are coping strategies and support available for pancreatic cancer patients and their caregivers. Support groups, counseling services, and self-care practices can help individuals navigate the emotional, physical, and practical challenges associated with the disease.
What advances in research and promising therapies are being made for pancreatic cancer ascites?
Ongoing research is exploring potential targeted therapies and emerging treatment approaches for pancreatic cancer ascites. Clinical trials and advancements in personalized medicine offer hope for improved outcomes and increased life expectancy.
How can lifestyle measures positively impact the well-being of individuals with pancreatic cancer ascites?
Adopting a balanced diet, engaging in regular exercise, managing stress, and exploring complementary therapies can positively impact the overall well-being of individuals with pancreatic cancer ascites.
Why is effective communication with healthcare professionals important in managing pancreatic cancer ascites?
Effective communication with healthcare professionals is crucial in managing pancreatic cancer ascites as it allows for shared decision-making, addressing concerns, and receiving the best possible care and support.
What is the emotional and psychological impact of pancreatic cancer and ascites?
Pancreatic cancer and ascites can have a significant emotional and psychological impact, leading to anxiety, depression, and grief. Seeking professional support and utilizing coping strategies are essential for maintaining emotional well-being.
Are there any patient stories and inspiring journeys related to pancreatic cancer ascites?
Yes, there are inspiring stories of individuals who have faced pancreatic cancer ascites. These stories provide personal insights into their experiences, treatments, and coping strategies, offering hope and motivation to others on a similar journey.
Are there supportive resources available for individuals with pancreatic cancer ascites?
Yes, there are supportive resources available for individuals with pancreatic cancer ascites. Reputable websites, organizations, helplines, and support groups offer valuable information, assistance, and emotional support to those affected by the disease.
How can patients empower themselves and improve their quality of life?
Patients can empower themselves by understanding their condition, actively participating in their care, seeking appropriate treatment and support, and maintaining a positive outlook. Staying informed about advancements in pancreatic cancer management is also important.