Prostate cancer is one of the most common cancers affecting men worldwide, and while many cases are detected early and remain localized, there are instances where the disease can spread beyond the prostate. Understanding where prostate cancer spreads and how it progresses is crucial for early detection, timely treatment, and better patient outcomes.
For men and their families, learning about the potential pathways of prostate cancer can reduce anxiety and provide clarity when discussing treatment options with healthcare providers. This article explores in detail the definition, causes, risk factors, symptoms, diagnostic methods, treatment strategies, prevention, and support for those dealing with prostate cancer.
Definition and Overview
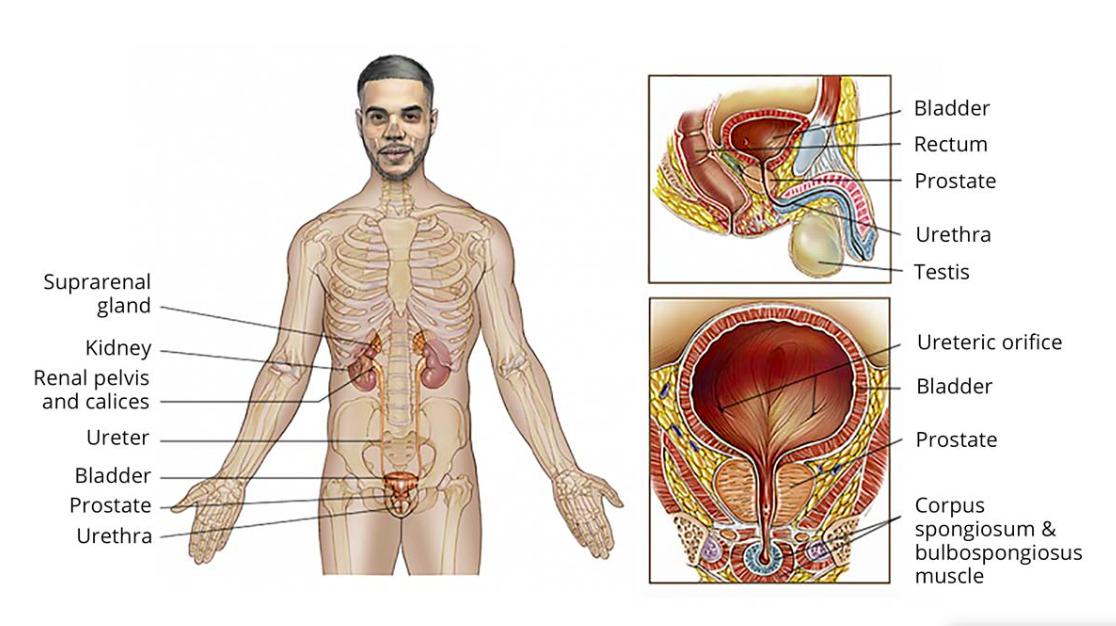
Prostate cancer begins in the prostate gland, a small walnut-shaped organ located below the bladder and in front of the rectum. It is responsible for producing seminal fluid, which nourishes and transports sperm. When abnormal cells in the prostate grow uncontrollably, prostate cancer develops.
In many cases, prostate cancer is slow-growing and confined to the gland. However, aggressive types can metastasize, meaning they spread to other parts of the body. The most common question patients ask is: where does prostate cancer spread? The typical areas include the bones, lymph nodes, liver, and lungs.
Types of Prostate Cancer
There are different types of prostate cancer, with adenocarcinoma being the most common. Other less common types include small cell carcinoma, neuroendocrine tumors, and transitional cell carcinoma. These rare types are often more aggressive and more likely to spread quickly.
Causes and Risk Factors
While the exact cause of prostate cancer is unknown, several risk factors increase the likelihood of developing the disease:
- Age: Men over 50 are at higher risk.
- Family history: Having a father or brother with prostate cancer significantly increases risk.
- Genetics: Inherited gene mutations, such as BRCA1 and BRCA2, may play a role.
- Race: African American men face a higher risk and often develop more aggressive forms.
- Diet and lifestyle: High-fat diets, obesity, and low physical activity may contribute to risk.
Symptoms and Early Warning Signs
In its early stages, prostate cancer may not cause noticeable symptoms. However, as the disease progresses, symptoms may include:
- Difficulty urinating or weak urine flow
- Frequent urination, especially at night
- Blood in urine or semen
- Erectile dysfunction
- Pain in the pelvic area or lower back
When prostate cancer spreads, additional symptoms may appear depending on the affected area, such as bone pain, swelling in the legs, or unexplained weight loss.
Diagnosis
Early detection plays a key role in improving outcomes. Common diagnostic methods include:
- Prostate-Specific Antigen (PSA) test: A blood test measuring PSA levels.
- Digital Rectal Exam (DRE): A physical examination of the prostate.
- Biopsy: Tissue sampling to confirm cancer.
- Imaging tests: MRI, CT scans, and bone scans help determine where prostate cancer spreads in advanced stages.
Treatment Options
Treatment depends on the stage, type, and spread of cancer. Options include:
- Active surveillance: Monitoring slow-growing cancers.
- Surgery: Removal of the prostate (prostatectomy).
- Radiation therapy: Targeting cancer cells with high-energy rays.
- Hormone therapy: Reducing or blocking testosterone that fuels cancer growth.
- Chemotherapy and immunotherapy: Used in advanced or aggressive cases.
Prevention and Lifestyle Recommendations
Although prostate cancer cannot always be prevented, lifestyle choices can reduce risk:
- Maintain a healthy diet rich in fruits, vegetables, and whole grains.
- Exercise regularly to manage weight and boost overall health.
- Limit red meat and processed foods.
- Attend regular screenings, especially if you are at high risk.
Prognosis and Survival Rates
The prognosis for prostate cancer depends on how early it is detected and whether it has spread. Localized prostate cancer has a very high survival rate, with many men living long, healthy lives. Once it spreads to distant organs, survival rates decrease, but advances in treatment continue to improve patient outcomes.
Latest Research and Innovations
Research into prostate cancer is ongoing, with new therapies such as targeted treatments, genetic testing, and precision medicine showing promise. Immunotherapy and advanced imaging techniques are also enhancing the ability to detect and manage metastatic prostate cancer.
Coping and Support for Patients
A prostate cancer diagnosis can be emotionally overwhelming. Patients and families are encouraged to seek support from:
- Professional counseling or therapy
- Patient support groups
- Educational resources provided by hospitals and cancer organizations
- Open communication with healthcare providers about treatment options and side effects
Conclusion
Understanding where does prostate cancer spread and how it develops is vital for patients, caregivers, and healthcare providers. While not all prostate cancers are aggressive, knowing the signs, risks, and pathways can make a significant difference in managing the disease. Early detection, informed decision-making, and lifestyle choices remain key to improving survival and quality of life.
FAQ
1. Where does prostate cancer spread first?
It usually spreads to the bones and nearby lymph nodes before reaching other organs.
2. Can prostate cancer spread to the liver or lungs?
Yes, in advanced stages, prostate cancer can metastasize to the liver, lungs, and other distant organs.
3. How fast does prostate cancer spread?
The speed varies. Some types are slow-growing, while aggressive forms can spread rapidly.
4. Can prostate cancer be cured if it spreads?
While cure rates are lower once it spreads, treatments can control the disease, relieve symptoms, and extend life.
5. What lifestyle changes can help reduce the risk?
Healthy eating, regular exercise, weight management, and regular screenings are highly recommended.