Pancreatic cancer is one of the most challenging cancers to diagnose and treat due to its aggressive nature and late detection in many patients. For those eligible, surgery provides the best chance of long-term survival, but outcomes vary depending on the stage of cancer, overall health, and treatment approach. Understanding the pancreatic cancer survival rate after surgery is essential for patients and their families to make informed decisions about treatment and lifestyle adjustments.
While the statistics can be daunting, advances in surgical techniques, chemotherapy, and targeted therapies are improving survival outcomes. With proper medical care, supportive resources, and awareness of risk factors, patients can improve their quality of life and potentially extend their survival. This article will explore the definition, symptoms, diagnosis, treatment, prognosis, and innovations in pancreatic cancer care with a focus on survival rates after surgery.
Definition and Overview
Pancreatic cancer begins when malignant cells form in the tissues of the pancreas, an organ located behind the stomach that plays a crucial role in digestion and blood sugar regulation. Because it often grows silently without symptoms, pancreatic cancer is usually diagnosed at an advanced stage, making it difficult to treat effectively.
Surgery, particularly the Whipple procedure (pancreaticoduodenectomy), is the most common curative treatment for localized pancreatic cancer. However, only a fraction of patients are eligible for surgery since many are diagnosed after the disease has spread.
Types
Pancreatic cancer is generally divided into two main categories:
- Exocrine tumors: The most common type, including pancreatic ductal adenocarcinoma, which accounts for over 90% of cases.
- Endocrine tumors (neuroendocrine tumors): Rare cancers that begin in hormone-producing cells of the pancreas.
Causes and Risk Factors
The exact cause of pancreatic cancer is not fully understood, but several factors can increase risk, including:
- Family history of pancreatic or related cancers
- Smoking and excessive alcohol use
- Chronic pancreatitis
- Obesity and poor diet
- Diabetes
- Genetic mutations such as BRCA1 and BRCA2
Symptoms and Early Warning Signs
Early symptoms are often vague and easily mistaken for other conditions. Some warning signs include:
- Abdominal or back pain
- Unexplained weight loss
- Jaundice (yellowing of the skin and eyes)
- Loss of appetite
- Nausea and digestive issues
- New-onset diabetes
Diagnosis
Diagnosing pancreatic cancer typically involves a combination of:
- Imaging tests such as CT scans, MRI, or PET scans
- Endoscopic ultrasound and biopsy for tissue confirmation
- Blood tests for tumor markers like CA 19-9
- Genetic testing for hereditary cancer syndromes
Treatment Options
Treatment depends on the stage of cancer and overall health of the patient. Common approaches include:
- Surgery: Whipple procedure, distal pancreatectomy, or total pancreatectomy
- Chemotherapy: Often given before or after surgery to kill remaining cancer cells
- Radiation therapy: Used in combination with other treatments
- Targeted therapy and immunotherapy: For patients with specific genetic mutations
- Palliative care: To manage symptoms and improve quality of life
Prevention and Lifestyle Recommendations
While not all cases of pancreatic cancer are preventable, certain lifestyle choices can reduce risk:
- Quit smoking and limit alcohol intake
- Maintain a healthy weight
- Eat a balanced diet rich in fruits, vegetables, and whole grains
- Exercise regularly
- Manage diabetes and chronic pancreatitis with proper medical care
Prognosis and Survival Rates
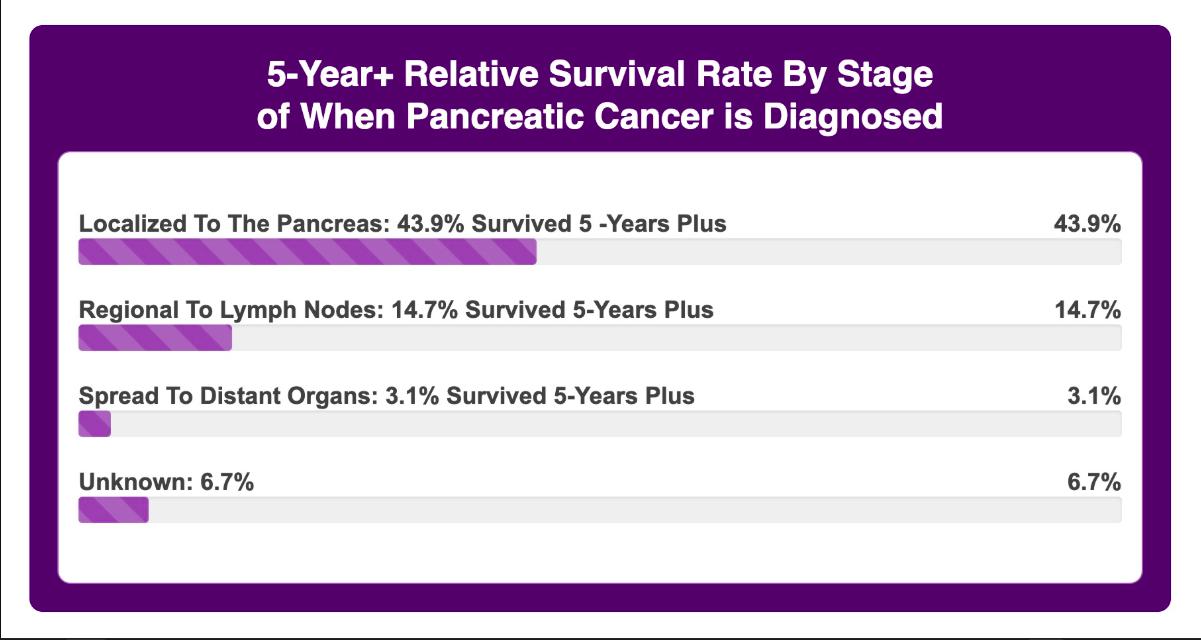
The pancreatic cancer survival rate after surgery varies greatly. On average:
- The five-year survival rate after surgery ranges from 20% to 30% for patients with localized disease.
- If the cancer is caught early and completely removed, survival rates may be higher.
- For advanced stages, the survival rate decreases significantly, even after surgery.
Other factors influencing survival include the patient’s age, response to chemotherapy, and genetic profile of the tumor. It is important to note that every case is unique, and survival statistics are only general estimates.
Latest Research and Innovations
Recent advancements are improving survival rates and treatment outcomes:
- Minimally invasive surgical techniques that reduce recovery time and complications
- Personalized medicine using genetic profiling to guide targeted therapy
- Immunotherapy trials that boost the body’s immune response to cancer cells
- Early detection biomarkers under investigation to diagnose pancreatic cancer before it spreads
Coping and Support for Patients
A diagnosis of pancreatic cancer can be overwhelming, both physically and emotionally. Patients benefit from:
- Support groups and counseling for emotional well-being
- Nutritional guidance to maintain strength during treatment
- Pain management and palliative care for symptom relief
- Family and caregiver support to navigate daily challenges
Conclusion
Pancreatic cancer remains one of the most aggressive forms of cancer, but surgery offers the best chance of long-term survival for eligible patients. The pancreatic cancer survival rate after surgery is improving thanks to advancements in medical research, targeted therapies, and comprehensive patient care. By focusing on early detection, lifestyle changes, and support systems, patients and families can face this journey with strength and hope.
FAQ
1. What is the average survival rate after pancreatic cancer surgery?
The five-year survival rate is around 20% to 30% for patients with localized pancreatic cancer who undergo surgery.
2. Can pancreatic cancer be cured with surgery?
Surgery can potentially cure pancreatic cancer if it is detected early and fully removed, but recurrence is common.
3. What type of surgery is most common for pancreatic cancer?
The Whipple procedure (pancreaticoduodenectomy) is the most common surgery for pancreatic cancer.
4. Does chemotherapy improve survival rates after surgery?
Yes, chemotherapy is often used after surgery to kill remaining cancer cells and reduce the risk of recurrence.
5. How can I lower my risk of pancreatic cancer?
Maintaining a healthy lifestyle with a balanced diet, regular exercise, no smoking, and controlled alcohol consumption can reduce risk.