Bone health plays a critical role in the overall well-being of individuals, especially those living with or recovering from cancer. A bone density test for cancer is a vital diagnostic tool that helps detect bone loss or weakness, often associated with cancer itself or as a side effect of cancer treatments. Early detection of bone changes can significantly influence treatment plans and improve a patient’s quality of life.
As cancer treatments such as chemotherapy, radiation, or hormonal therapy can impact bone strength, regular bone density assessments are essential. These tests help oncologists monitor changes in bone mass, prevent fractures, and manage potential complications. Understanding how bone density testing relates to cancer care empowers patients and caregivers to make informed medical decisions.
Definition and Overview
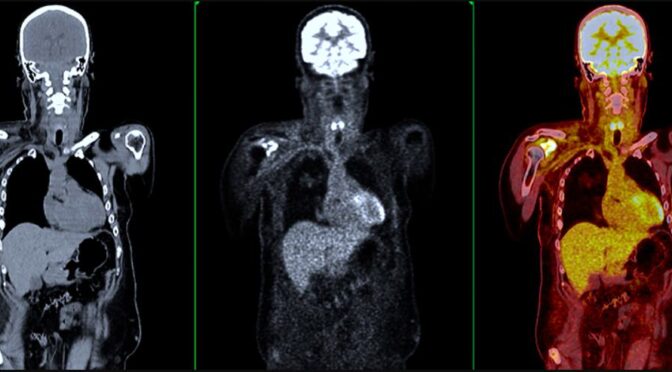
A bone density test for cancer—also known as a DEXA scan (Dual-Energy X-ray Absorptiometry)—is a non-invasive imaging procedure that measures bone mineral density (BMD). The test determines how strong the bones are and whether bone loss (osteopenia or osteoporosis) is present. In cancer patients, this test is used not only to evaluate general bone health but also to detect metastasis, especially in cancers that tend to spread to the bones such as breast, prostate, and lung cancers.
The results are usually expressed as a T-score, which compares a patient’s bone density with that of a healthy young adult. A lower score indicates weaker bones and higher fracture risk.
Types of Bone Density Tests
- DEXA (Dual-Energy X-ray Absorptiometry) Scan – The most common and accurate test for measuring bone density in the spine, hip, and forearm.
- Peripheral DEXA Scan – A smaller version that tests bone density in peripheral areas like the wrist or heel.
- Quantitative CT Scan – Provides 3D images and measures bone strength in the spine.
- Ultrasound Bone Densitometry – Uses sound waves to assess bone density, often as a preliminary screening tool.
Causes and Risk Factors
Bone loss or fragility in cancer patients can result from several causes, including:
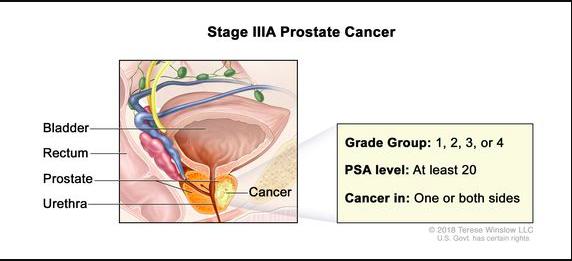
- Cancer metastasis to bones, especially from breast, prostate, or lung cancer
- Hormonal treatments, such as estrogen-blocking therapy for breast cancer or androgen deprivation for prostate cancer
- Chemotherapy side effects that interfere with calcium absorption or bone cell regeneration
- Steroid medications used to manage cancer symptoms
- Nutritional deficiencies, especially in calcium and vitamin D
- Physical inactivity, often due to fatigue or treatment recovery
Symptoms and Early Warning Signs
While bone loss is often silent, patients may experience:
- Persistent bone or joint pain
- Unexplained fractures or brittleness
- Back pain due to spinal compression fractures
- Loss of height or stooped posture
- Weakness or mobility challenges
Patients undergoing cancer treatment should promptly report these symptoms to their healthcare provider to determine whether a bone density test for cancer is necessary.
Diagnosis
During a bone density test for cancer, patients lie on a padded table while a scanner passes over the body, emitting low-dose X-rays. The procedure typically lasts about 10–20 minutes and is painless. The test results help doctors:
- Assess the risk of bone fractures
- Detect early signs of osteoporosis or metastasis
- Evaluate the effectiveness of cancer therapy on bone health
- Adjust treatment plans to protect and strengthen bones
Treatment Options
If bone loss or cancer-related bone disease is detected, treatment may include:
- Bisphosphonates or Denosumab to strengthen bones and reduce fracture risk
- Calcium and vitamin D supplements to improve bone density
- Hormonal therapy adjustments to reduce bone degradation
- Targeted radiation therapy for bone metastases
- Pain management strategies and physiotherapy to maintain mobility
Prevention and Lifestyle Recommendations
Maintaining strong bones is crucial for cancer patients. Preventive strategies include:
- Consuming a calcium- and vitamin D-rich diet (e.g., dairy, leafy greens, fortified foods)
- Engaging in weight-bearing exercises like walking or light resistance training
- Limiting alcohol and avoiding smoking
- Managing hormone levels under medical supervision
- Getting regular bone density tests as recommended by your oncologist
Prognosis and Survival Rates
Bone complications can influence cancer outcomes and patient quality of life. However, with early detection through a bone density test for cancer, bone loss and metastasis can often be managed effectively. Treatments can stabilize bone health, reduce pain, and extend survival rates, especially when integrated into a comprehensive cancer care plan.
Latest Research and Innovations
Recent research highlights the growing importance of AI-driven bone imaging and biomarker-based bone monitoring in cancer care. New medications like osteoprotective agents are being developed to specifically target bone metastases. Researchers are also exploring genetic markers to predict which cancer patients are most at risk for bone-related complications, allowing for more personalized treatment strategies.
Coping and Support for Patients
Living with cancer-related bone issues can be emotionally and physically challenging. Patients are encouraged to seek:
- Support groups and counseling services
- Rehabilitation programs to rebuild strength and mobility
- Nutritional counseling to promote bone health
- Regular communication with healthcare teams for ongoing monitoring
Emotional resilience and a strong support system can greatly improve a patient’s ability to cope with treatment and recovery.
Conclusion
A bone density test for cancer is more than just a diagnostic tool—it’s a key component of comprehensive cancer care. Regular testing helps detect early bone loss, prevent fractures, and manage metastasis effectively. With advances in medical imaging and targeted therapies, cancer patients today have better chances of maintaining strong bones and improving long-term outcomes.
Frequently Asked Questions (FAQ)
1. What is a bone density test for cancer?
It’s a non-invasive imaging test that measures bone mineral density to detect bone loss or cancer spread to bones.
2. Why do cancer patients need a bone density test?
Because certain cancer treatments and metastases can weaken bones, increasing fracture risk.
3. Is the bone density test painful?
No, it’s a simple and painless scan that usually takes less than 20 minutes.
4. How often should cancer patients have this test?
It depends on the type of cancer and treatment plan, but usually once a year or as advised by your doctor.
5. Can bone loss from cancer be reversed?
While complete reversal is rare, proper treatment and lifestyle changes can significantly improve bone strength and reduce complications.