Stagescancer.net – For patients with multiple myeloma, a diagnosis can be overwhelming. The good news is that stem cell transplantation has been proven effective in extending life expectancy, providing hope for those with this cancer of the plasma cells that impact the bone marrow. This article will provide an overview of multiple myeloma life expectancy after stem cell transplant, including the post-treatment outlook, factors that influence survival rates, and the latest research and advances in this field.
Understanding Multiple Myeloma
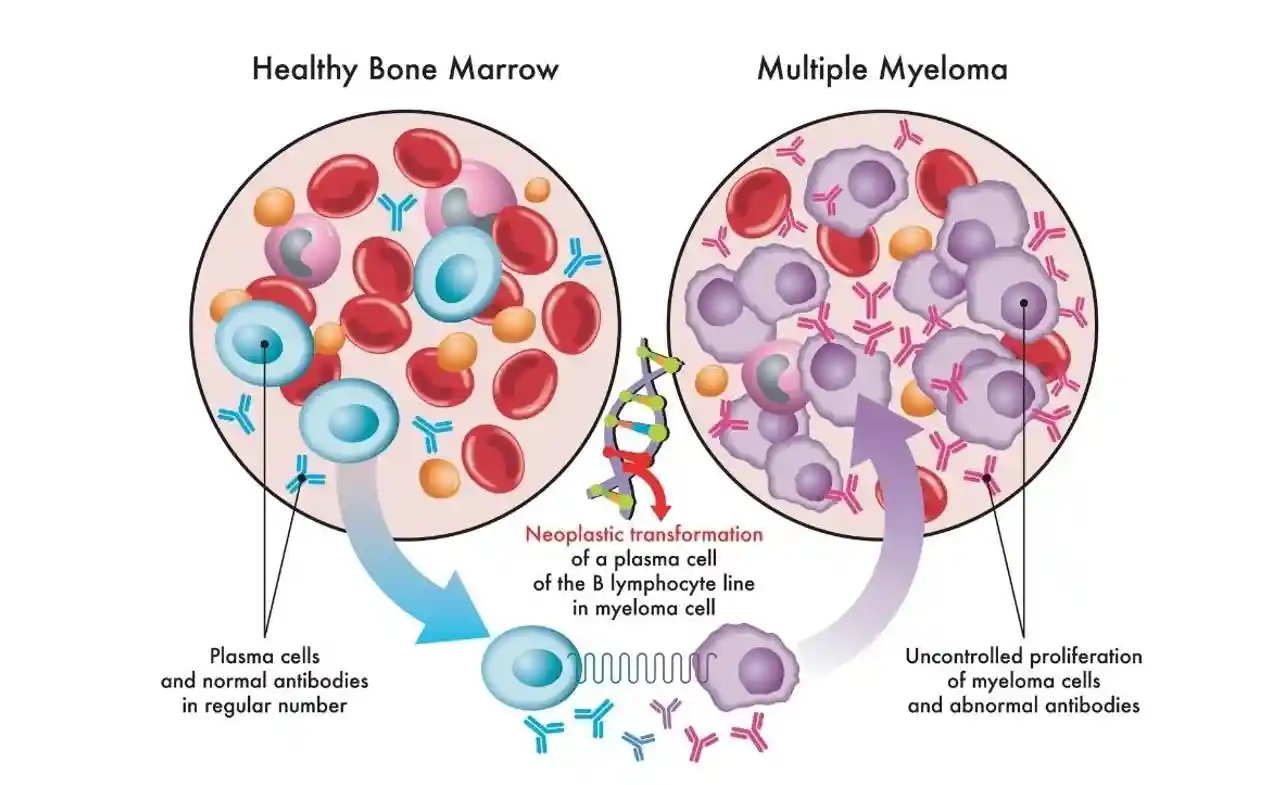
Multiple myeloma is a type of cancer that forms in plasma cells, which are white blood cells that produce antibodies. This disease is characterized by the abnormal growth and accumulation of these cells in the bone marrow, which can lead to bone pain, weakened bones, and an increased risk of fractures.
The abnormal plasma cells can also produce abnormal proteins that can lead to kidney damage and other complications. Multiple myeloma is a complex disease that affects each person differently, and its treatment requires a personalized approach.
Patients diagnosed with multiple myeloma will undergo a series of tests to determine the extent of the disease and its specific genetic features. This information is used to guide treatment decisions and improve outcomes.
The treatment of multiple myeloma may involve a combination of chemotherapy, immunotherapy, targeted therapies, and, in some cases, stem cell transplantation. In the following sections, we will explore the various treatment options available for multiple myeloma and the factors that can impact a patient’s post-treatment outlook.
Introduction to Stem Cell Transplantation
Stem cell transplantation, or SCT, is a treatment option for multiple myeloma. It involves replacing damaged or destroyed cells in the bone marrow with healthy cells, known as stem cells.
Types of Stem Cell Transplantation
There are two main types of SCT: autologous transplant and allogeneic transplant.
| Type | Description |
|---|---|
| Autologous transplant | Uses the patientwn stem cells, collected before undergoing chemotherapy or radiation therapy. This type of transplant reduces the risk of complications and side effects associated with allogeneic transplants. |
| Allogeneic transplant | Uses stem cells from a donor, which are matched to the patient’s tissue type. The donor’s immune system also replaces the patient’s immune system. This type of transplant has a higher risk of complications due to the possibility of rejection or graft-versus-host disease. |
Patients who undergo SCT receive a high dose of chemotherapy and, in some cases, radiation therapy before the transplant. This is known as a conditioning regimen, and it eliminates cancerous cells and prepares the patient’s body for the transplant.
After the conditioning regimen, patients receive a stem cell infusion, which reintroduces the healthy stem cells into the body. These stem cells then grow and replace the cells damaged by the conditioning regimen, promoting recovery and remission of the disease.
Factors Affecting Multiple Myeloma Life Expectancy
Multiple myeloma is a complex disease, and several factors can impact a patient’s life expectancy post-treatment. Age, disease stage, and genetic factors play a significant role in determining the likelihood of remission and survival.
Age is an essential factor in multiple myeloma life expectancy. Elderly patients may have reduced treatment tolerance and higher susceptibility to complications, which can impact post-transplant outcomes. Disease stage is another critical determinant, as patients diagnosed with later-stage multiple myeloma may have a poorer prognosis.
Genetic factors can also play a vital role in multiple myeloma life expectancy. The presence of certain mutations or genetic abnormalities can increase the risk of relapse or disease progression.
It is crucial to consider these factors when assessing post-transplant outlook for patients with multiple myeloma. Adequate monitoring and follow-up care are necessary to ensure early detection of any potential complications or disease relapse.
Stem Cell Transplant Process
The stem cell transplant process is a critical component of treatment for multiple myeloma. It involves several steps, starting with a conditioning regimen designed to prepare the body for the stem cell infusion.
Conditioning Regimen
The conditioning regimen typically involves chemotherapy drugs and, in some cases, radiation therapy. The purpose of this regimen is to destroy any remaining cancer cells in the body and to create a clean slate for the new stem cells to take hold. The duration and intensity of the conditioning regimen varies, depending on the patient’s specific needs and overall health.
Stem Cell Infusion
Once the conditioning regimen is complete, the stem cell infusion can take place. In an autologous transplant, the patient’s stem cells are collected before the conditioning regimen, treated to remove any remaining cancer cells, and then reinfused back into the patient’s body. In an allogeneic transplant, the stem cells come from a donor and must be a good match for the patient. The stem cells are typically administered through a catheter, and the procedure is typically performed on an outpatient basis.
After the stem cell infusion, the patient will undergo a period of close monitoring to ensure that the new stem cells take hold and begin to produce healthy blood cells. During this time, which typically lasts several weeks, the patient may be at increased risk for infections and other complications.
Immediate Post-Transplant Recovery
Following a stem cell transplant, patients enter into the immediate post-transplant recovery phase. During this time, it is critical to monitor for any potential complications and side effects that may arise.
Patients may experience a range of side effects during this phase, such as nausea, vomiting, and fatigue. They may also be at risk of infection due to a weakened immune system. Careful monitoring and management of symptoms are essential for a successful recovery.
Complications may also arise, such as graft-versus-host disease (GVHD) in allogeneic transplants. GVHD occurs when the transplanted cells attack the recipient’s healthy tissues and organs. It can lead to serious health problems and require additional treatment. Close observation and early intervention are crucial in addressing these complications.
Early Post-Transplant Period
Following the stem cell transplant, patients enter the early post-transplant period, which is a critical phase in their recovery. During this time, the immune system is severely compromised, leaving patients vulnerable to infection, and requiring close monitoring by medical professionals. It is essential to maintain a sterile environment, take appropriate precautions, and ensure prompt treatment for any signs of infection.
The early post-transplant period is also marked by the gradual recovery of the immune system. The body works to rebuild blood counts and other key metrics that have been suppressed by the conditioning regimen. This recovery process can take several weeks or even months, and patients should take steps to strengthen their immune system through careful nutrition, hydration, and exercise.
Immune System Recovery
The recovery of the immune system is a gradual and complex process that requires close attention to specific parameters. Doctors will monitor the patient’s white blood cell counts, neutrophil counts, and other metrics to ensure that their immune system is recovering appropriately. Patients may receive medications to help strengthen their immune system and to stimulate blood cell growth.
Follow-up Care
After the stem cell transplant procedure, patients will undergo extensive follow-up care and monitoring to ensure a successful recovery. Careful monitoring of the immune system and blood counts, as well as routine assessments of the patient’s vital signs, are essential during the early post-transplant period. Follow-up care typically involves regular appointments with the hematologist/oncologist, as well as other medical professionals.
The early post-transplant period can be challenging, and patients should expect to experience some side effects, such as fatigue, nausea, and hair loss. However, with proper care and monitoring, many patients can recover from the transplant and enjoy a good quality of life. Patients should work closely with their medical team to manage any complications that arise during this period and to receive the support and interventions needed to promote their overall well-being.
Long-Term Follow-Up and Monitoring
Long-term follow-up and monitoring are crucial for individuals who have undergone a stem cell transplant for multiple myeloma. The risk of disease recurrence always exists, and just because a patient is in remission, it doesn’t mean they can ignore continuing with regular monitoring.
Persistent monitoring is essential to detect any signs of disease recurrence early on. A relapse, if detected, can be treated more effectively if caught in the early stages. On the other hand, if recurrence happens later on, treatment regimens might be more aggressive and pose more significant risks to the patient.
While regular monitoring is usually done in the first two years following the transplantation procedure, ongoing assessments afterward are vital. Doctors recommend check-ups at least once a year, and some patients may need more frequent follow-ups, depending on their individual circumstances.
The Role of Imaging and Blood Tests
Monitoring multiple myeloma after a stem cell transplant requires a combination of imaging scans and blood tests. These tests are important to detect any early signs of relapse and monitor patients for any complications, such as graft-versus-host disease.
| Imaging Tests | Blood Tests |
|---|---|
| Computed Tomography (CT) Scan | Blood Urea Nitrogen (BUN) |
| Magnetic Resonance Imaging (MRI) | Creatinine |
| Positron Emission Tomography (PET) Scan | Liver Function Tests (LFTs) |
PET scans are particularly good at detecting early signs of relapse, while MRI scans help to detect bone damage or disease in other areas of the body. Blood tests are also essential to monitor the patient’s overall health and detect any abnormalities in blood cell count, kidney function, or liver enzymes.
It’s essential to work closely with healthcare providers to determine an individualized monitoring schedule while keeping track of all test results over time. A well-organized and tracked record of monitoring can help medical teams predict potential problems and address them before they become serious.
Overall, long-term follow-up and monitoring represent significant milestones post stem cell transplantation. It’s crucial to follow instructions from healthcare providers and undergo routine testing as suggested.
Factors Influencing Post-Transplant Life Expectancy
Post-transplant life expectancy for individuals with multiple myeloma is influenced by various factors. One of the most significant factors is disease response, specifically achieving deep and sustained remission. Research has found that patients who achieve this type of remission have better outcomes and longer life expectancy.
Other important factors to consider include disease stage, age at diagnosis, and genetic factors. Patients diagnosed at an earlier stage typically have better outcomes post-transplant. Similarly, younger patients tend to fare better than older patients. Genetic factors, such as chromosomal abnormalities, can also impact post-transplant life expectancy.
It’s essential to consider these factors when assessing a patient’s post-transplant outlook. Working closely with a healthcare team can help ensure that patients receive the most appropriate treatment and support post-transplant.
Prognostic Factors for Post-Transplant Survival
Prognostic factors play a critical role in determining the survival rates of individuals with multiple myeloma post-transplant. Cytogenetics, an analysis of the chromosomes in cancer cells, is an important prognostic factor. Patients with certain chromosomal abnormalities may have a poorer prognosis. Additionally, minimal residual disease (MRD), or the presence of small amounts of cancer cells after treatment, can also influence post-transplant survival rates. Patients who achieve a deep and sustained remission have a better prognosis.
Other factors that can impact survival rates include age, disease stage, and overall health status. Advanced age and more advanced disease stage at the time of transplant may lead to lower survival rates.
| Prognostic Factors | Impact on Survival Rate |
|---|---|
| Cytogenetics | May negatively impact survival rates |
| Minimal Residual Disease (MRD) | Presence of MRD may negatively impact survival rates |
| Age | Advanced age may lead to lower survival rates |
| Disease Stage | More advanced disease stage may lead to lower survival rates |
| Overall Health Status | Poor overall health may lead to lower survival rates |
Understanding these prognostic factors can help healthcare providers predict post-transplant survival rates and develop treatment plans that are tailored to individual patients’ needs and risk factors.
Research and Advances in Stem Cell Transplantation
Stem cell transplantation for multiple myeloma has seen significant advancements in recent years, thanks to ongoing research and clinical trials. These studies are aimed at improving outcomes and developing novel therapies to further enhance life expectancy.
One area of focus is the use of targeted therapies, which work to attack cancer cells while sparing healthy ones. One such therapy is chimeric antigen receptor (CAR) T-cell therapy, which harnesses the power of the immune system to target cancer cells. Trials have shown promising results, with some patients achieving deep and sustained remission.
Another area of research is in the use of second-line treatments for patients who experience disease relapse after initial treatment. Studies are exploring the use of repeated stem cell transplantation, as well as new drug combinations, to improve outcomes in these cases.
Other promising advances in stem cell transplantation for multiple myeloma include:
- Improved conditioning regimens to reduce toxicity and improve engraftment
- Innovative graft engineering techniques to reduce the risk of relapse
- Expanded use of haploidentical transplantation, which allows stem cell transplant from half-matched donors
These advancements represent significant progress in the field of stem cell transplantation for multiple myeloma, offering hope for improved outcomes and enhanced life expectancy for patients.
Supportive Care Post-Transplant
Supportive care is crucial for patients after a stem cell transplant. Post-transplant, patients may experience physical, emotional, and psychological challenges that require careful attention to improve their quality of life. Supportive care measures can include:
- Management of pain and other symptoms
- Prevention and treatment of infections
- Dietary and nutritional support
- Physical therapy and rehabilitation
- Emotional and psychological support
Patients may also benefit from participating in support groups or counseling to cope with the stress and uncertainty of their diagnosis and treatment. Supportive care interventions can make a significant difference in patients’ overall well-being and should be a critical part of comprehensive post-transplant care.
Survivorship and Coping Strategies
Undergoing a stem cell transplant for multiple myeloma can take a toll on emotional well-being. Coping with the stress and anxiety that come with the procedure can be challenging, but developing effective strategies can make a significant difference in survivorship.
One coping strategy is to maintain a positive mindset. Research has shown that optimistic individuals tend to have better health outcomes and faster recovery rates. Practicing mindfulness, engaging in relaxing activities, and seeking distraction through hobbies or social activities are all ways to stay positive.
Another important strategy for coping is seeking support. Emotional support from loved ones can help alleviate stress and provide a sense of comfort during difficult times. Mental health professionals, support groups, and online communities can also offer valuable resources for those going through the transplant process.
Maintaining a healthy lifestyle is also essential for promoting emotional well-being and survivorship. Regular exercise, a balanced diet, and quality sleep can all help manage stress and improve overall health and well-being.
Coping Strategies for Post-Transplant Survivorship
| Coping Strategy | Description |
|---|---|
| Positive mindset | Practicing optimism and mindfulness, engaging in relaxing activities, and seeking distraction through hobbies or social activities. |
| Seeking support | Emotional support from loved ones, mental health professionals, support groups, and online communities. |
| Healthy lifestyle | Regular exercise, a balanced diet, and quality sleep. |
Developing effective coping strategies is an important component of survivorship for individuals who have undergone a stem cell transplant for multiple myeloma. By prioritizing self-care, seeking support, and maintaining a positive mindset, individuals can enhance emotional well-being and improve their overall quality of life.
Conclusion
Post-transplant life expectancy is a critical consideration for individuals with multiple myeloma. While many factors can influence the outcome, stem cell transplantation provides a promising avenue for improving survival rates and achieving long-term disease control.
Understanding the disease and the transplant process, as well as identifying prognostic factors, can help inform treatment decisions and optimize outcomes. Equally important are the supportive care measures and coping strategies that can enhance quality of life and emotional well-being post-transplant.
As research continues to advance in the field of stem cell transplantation, new therapies and approaches will likely emerge, further improving outcomes for individuals with multiple myeloma. While the journey is not easy, those who undergo a stem cell transplant for multiple myeloma have reason to be hopeful for the future.
FAQ
What is multiple myeloma?
Multiple myeloma is a type of cancer that affects plasma cells, which are a type of white blood cell found in the bone marrow.
What is a stem cell transplant?
A stem cell transplant is a medical procedure in which healthy stem cells are infused into a patient’s body to replace damaged or diseased cells.
What are the different types of stem cell transplantation?
There are two main types of stem cell transplantation: autologous transplant, which uses the patient’s own stem cells, and allogeneic transplant, which uses stem cells from a donor.
What factors can influence the life expectancy of individuals with multiple myeloma?
Several factors can affect the life expectancy of individuals with multiple myeloma, including age, disease stage, and genetic factors.
What is the process of a stem cell transplant?
The stem cell transplant process involves a conditioning regimen, which includes chemotherapy and sometimes radiation, followed by the infusion of stem cells.
What are the immediate post-transplant recovery periods?
The immediate post-transplant recovery period is a critical phase where patients need to be closely monitored for potential complications and side effects.
What is the early post-transplant period?
The early post-transplant period is when patients’ immune systems start to recover, and they receive follow-up care to monitor their progress and provide support.
Why is long-term follow-up and monitoring important after a stem cell transplant?
Long-term follow-up and monitoring are crucial to detect any disease recurrence and address any late effects or complications that may arise post-transplant.
What factors can influence post-transplant life expectancy?
Factors such as disease response and achieving remission can have an impact on post-transplant life expectancy for individuals with multiple myeloma.
What prognostic factors are considered for post-transplant survival?
Prognostic factors, such as cytogenetics and minimal residual disease (MRD), play a role in predicting post-transplant survival rates for patients.
What are the latest research and advances in stem cell transplantation for multiple myeloma?
Ongoing research aims to improve outcomes by exploring novel therapies and advancements in stem cell transplantation for multiple myeloma.
What supportive care measures are available for patients post-transplant?
There are various supportive care interventions and strategies that can contribute to improved quality of life and overall well-being for patients post-transplant.
How can individuals cope with survivorship after a stem cell transplant for multiple myeloma?
Coping strategies, such as maintaining a positive mindset and seeking support, can help individuals navigate the emotional challenges of survivorship after a stem cell transplant.
What are the key takeaways regarding post-transplant life expectancy for individuals with multiple myeloma?
Post-transplant life expectancy for individuals with multiple myeloma is influenced by numerous factors and requires consideration of various aspects, including the disease response and the achievement of sustained remission.