Stagescancer.net – Cancer, a complex and multifaceted disease, affects millions of people worldwide. With advancements in research and technology, targeted therapy has emerged as a promising approach to combat specific types of cancer. Tyrosine kinase cancer, characterized by abnormalities in tyrosine kinase activity, is one such subtype where targeted therapies have shown remarkable efficacy.
Tyrosine kinases are enzymes that play a critical role in various cellular processes, including cell growth, proliferation, and survival. However, when these kinases become dysregulated, they can drive the development and progression of cancer. Targeted therapy aims to inhibit the abnormal activity of these kinases, thereby halting the growth of cancer cells while sparing healthy tissues.
In this article, we will delve into the world of tyrosine kinase cancer targets and their role in targeted therapy. We will explore the different types of tyrosine kinase cancer, the mechanisms of action of tyrosine kinase inhibitors, and the challenges associated with this form of treatment. Furthermore, we will discuss the exciting developments in tyrosine kinase cancer research and the future directions of personalized medicine.
Join us on this journey as we unravel the intricate connections between tyrosine kinase cancer, targeted therapy, and the ongoing efforts to improve cancer treatment outcomes. Together, we can gain a deeper understanding of this field and pave the way for innovative approaches to combat cancer.
What is Tyrosine Kinase?
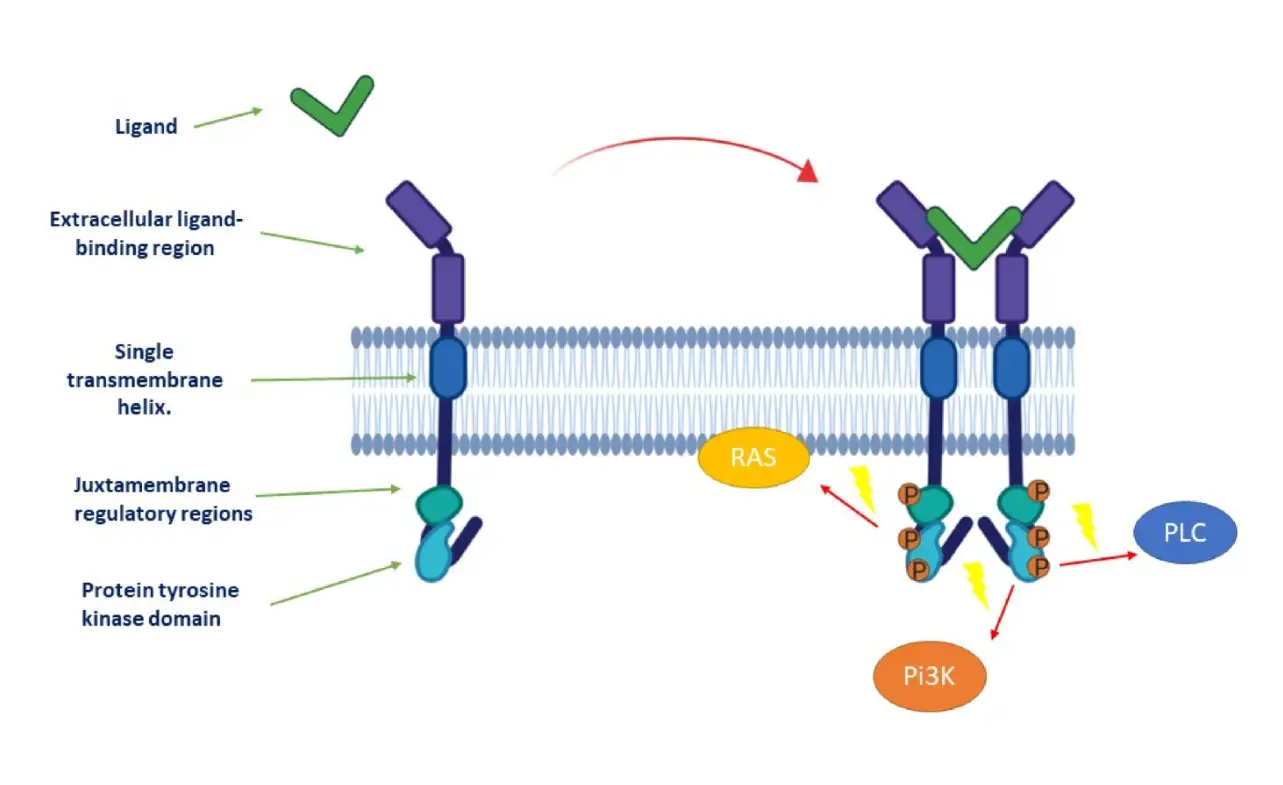
Tyrosine kinase is a type of enzyme that plays a critical role in cell signaling pathways. It regulates various cellular processes, including cell growth, division, and differentiation. Tyrosine kinases transfer a phosphate group from ATP to tyrosine residues in proteins, thereby activating or inactivating specific signaling molecules.
Abnormalities in tyrosine kinase activity can lead to dysregulated signaling pathways, contributing to the development and progression of cancer. Mutations or overexpression of tyrosine kinase genes can result in uncontrolled cell growth and survival, promoting tumor formation.
Understanding the role of tyrosine kinase in cancer is crucial for the development of targeted therapies that specifically inhibit its activity, aiming to disrupt the aberrant signaling and halt cancer progression.
| Type of Tyrosine Kinase | Associated Cancers |
|---|---|
| Fusion tyrosine kinases | Chronic myeloid leukemia (CML) |
| Epidermal growth factor receptor (EGFR) | Non-small cell lung cancer (NSCLC) |
| Platelet-derived growth factor receptor (PDGFR) | Gastrointestinal stromal tumors (GIST) |
| Anaplastic lymphoma kinase (ALK) | Non-small cell lung cancer (NSCLC) |
| Receptor tyrosine kinases (RTKs) | Breast cancer, colorectal cancer, and more |
Understanding the intricacies of tyrosine kinase activity and its role in cancer development is crucial for developing targeted therapies that specifically block tyrosine kinase activity and disrupt cancer signaling pathways.
Types of Tyrosine Kinase Cancer
Tyrosine kinase cancer encompasses a diverse range of malignancies that are characterized by abnormalities in the activity of tyrosine kinases, which are enzymes involved in cellular signaling pathways. These abnormalities can lead to uncontrolled cell growth and the development of cancer. Here, we examine two prominent types of tyrosine kinase cancer: chronic myeloid leukemia (CML) and non-small cell lung cancer (NSCLC).
Chronic Myeloid Leukemia (CML)
CML is a hematological malignancy that arises from a genetic alteration known as the Philadelphia chromosome. This chromosome results from a translocation between chromosomes 9 and 22, leading to the formation of the BCR-ABL fusion gene. The BCR-ABL fusion protein acts as a constitutively activated tyrosine kinase, driving the uncontrolled proliferation of myeloid cells in the bone marrow.
- Most common type of tyrosine kinase cancer
- Primarily affects adults, with a median age of diagnosis of around 50 years
- The initial chronic phase can progress to accelerated and blast phases if left untreated
- Treatment options include tyrosine kinase inhibitors, such as imatinib, dasatinib, and nilotinib
Non-Small Cell Lung Cancer (NSCLC)
NSCLC is the most common type of lung cancer, accounting for approximately 85% of all cases. Aberrant activity of tyrosine kinases, particularly those associated with epidermal growth factor receptor (EGFR), plays a significant role in the development and progression of NSCLC.
- Major subtypes of NSCLC include adenocarcinoma, squamous cell carcinoma, and large cell carcinoma
- EGFR mutations are present in approximately 15-20% of NSCLC cases, particularly in non-smokers and individuals of East Asian descent
- Targeted therapies, such as EGFR tyrosine kinase inhibitors (TKIs) like erlotinib, gefitinib, and osimertinib, have improved outcomes for patients with EGFR-mutated NSCLC
These are just two examples of tyrosine kinase cancer types, highlighting the significance of tyrosine kinase abnormalities in different malignancies. Further research continues to uncover additional tyrosine kinase-driven cancers and develop targeted therapies to effectively treat them.
Understanding Tyrosine Kinase Inhibitors
Tyrosine kinase inhibitors are a class of targeted therapy drugs that play a crucial role in the treatment of cancer. They work by blocking the activity of tyrosine kinases, which are enzymes involved in cell signaling pathways that regulate cell growth, division, and survival. Abnormalities in tyrosine kinase activity can lead to the development and progression of cancer.
These inhibitors specifically target the tyrosine kinases that are overactive or mutated in cancer cells, inhibiting their function and preventing the growth and spread of these cells. By targeting specific tyrosine kinases, these inhibitors minimize damage to healthy cells and reduce the side effects associated with traditional chemotherapy.
One of the key mechanisms of tyrosine kinase inhibitors is binding to the tyrosine kinase receptor’s ATP-binding site, preventing the phosphorylation of downstream signaling molecules and inhibiting the activation of signaling pathways that promote cancer cell growth and survival. This targeted approach has revolutionized cancer treatment and significantly improved patient outcomes.
Common Tyrosine Kinase Inhibitors
| Inhibitor | Target | Approved Indications |
|---|---|---|
| Imatinib (Gleevec) | BCR-ABL | Chronic Myeloid Leukemia (CML) |
| Erlotinib (Tarceva) | EGFR | Non-Small Cell Lung Cancer (NSCLC) |
| Dasatinib (Sprycel) | BCR-ABL, SRC | CML, Acute Lymphoblastic Leukemia (ALL) |
These are just a few examples of the tyrosine kinase inhibitors that have been approved by the FDA for the treatment of specific types of cancer. There are many more inhibitors in development and undergoing clinical trials, targeting various tyrosine kinases in different types of cancer.
While tyrosine kinase inhibitors have shown remarkable success in treating cancer, the development of resistance to these drugs remains a challenge. Cancer cells can acquire mutations or activate alternative signaling pathways that bypass the inhibition caused by these drugs, leading to treatment failure. Researchers are actively working on strategies to overcome resistance and improve the effectiveness of tyrosine kinase inhibitors.
FDA-Approved Tyrosine Kinase Inhibitors
Tyrosine kinase inhibitors (TKIs) have emerged as a revolutionary treatment option for various types of cancer. Over the years, the U.S. Food and Drug Administration (FDA) has approved several TKIs that specifically target aberrant tyrosine kinase activity in cancer cells. These FDA-approved TKIs have shown promising efficacy, offering renewed hope for patients battling these malignancies.
Here are some of the FDA-approved tyrosine kinase inhibitors:
| Drug Name | Type of Cancer | Efficacy | Potential Side Effects |
|---|---|---|---|
| Imatinib (Gleevec) | Chronic Myeloid Leukemia (CML) | High response rates, prolonged survival | Nausea, fatigue, muscle cramps |
| Erlotinib (Tarceva) | Non-Small Cell Lung Cancer (NSCLC) | Improved progression-free survival | Rash, diarrhea, fatigue |
| Ruxolitinib (Jakafi) | Myelofibrosis | Reduces spleen size, alleviates symptoms | Anemia, thrombocytopenia, dizziness |
These FDA-approved TKIs have demonstrated significant clinical benefits, including improved survival rates, enhanced quality of life, and better disease management. However, like any medication, they may also cause side effects that should be closely monitored and managed by healthcare professionals.
Further research and clinical trials are underway to explore the potential of other tyrosine kinase inhibitors in the treatment of various cancers. By targeting specific molecular alterations in cancer cells, FDA-approved TKIs pave the way for personalized and more effective cancer therapies.
Resistance to Tyrosine Kinase Inhibitors
Resistance to tyrosine kinase inhibitors (TKIs) is a significant challenge in the treatment of cancer patients. Although these targeted therapies have shown remarkable efficacy, the development of resistance can limit their long-term effectiveness.
Mechanisms of Resistance
The development of resistance to TKIs can occur through various mechanisms. One common mechanism is the acquisition of mutations in the target tyrosine kinase gene, rendering it less susceptible to inhibition by the drug. Additionally, alterations in downstream signaling pathways or the activation of compensatory growth factor receptors can also contribute to resistance.
Strategies to Overcome Resistance
Overcoming resistance to TKIs is a complex task that requires a comprehensive understanding of the underlying mechanisms. Researchers are actively exploring several strategies to address this challenge:
- Combination therapies: By combining different targeted therapies or combining a TKI with other treatment modalities, such as chemotherapy or immunotherapy, it may be possible to circumvent resistance mechanisms and improve treatment outcomes.
- Development of next-generation TKIs: Researchers are working to develop new generations of TKIs that can effectively target tyrosine kinases, including those with acquired mutations. These new drugs may provide improved efficacy and overcome resistance.
- Precision medicine: Personalized treatment approaches, based on genetic profiling of tumors, can help identify specific resistance mechanisms and guide the selection of targeted therapies that are more likely to be effective.
- Combating tumor heterogeneity: Tumors are often composed of a heterogeneous population of cells, some of which may be resistant to TKIs. Strategies that target multiple cell populations or the tumor microenvironment could help overcome resistance.
| Challenge | Strategy |
|---|---|
| Acquired mutations | Development of next-generation TKIs |
| Compensatory signaling | Combination therapies |
| Tumor heterogeneity | Targeting multiple cell populations or the tumor microenvironment |
| Lack of target specificity | Precision medicine |
By focusing on these strategies, researchers are dedicated to overcoming resistance to TKIs and improving the long-term outcomes for patients with tyrosine kinase-driven cancers.
Combining Tyrosine Kinase Inhibitors with Other Treatments
Combination therapy, which involves the simultaneous use of multiple treatment modalities, has emerged as a promising approach to cancer treatment. By combining tyrosine kinase inhibitors with other therapies, such as chemotherapy or immunotherapy, healthcare professionals aim to enhance response rates and improve patient outcomes.
The rationale behind combination therapy lies in the complementary mechanisms of action of different treatments. Tyrosine kinase inhibitors target specific pathways involved in cancer development and growth, while chemotherapy drugs aim to destroy rapidly dividing cancer cells. Immunotherapy, on the other hand, harnesses the power of the immune system to identify and eliminate cancer cells.
When used together, these treatments have the potential to create a synergistic effect, maximizing their benefits and increasing the likelihood of tumor response. These combinations can also address the issue of drug resistance, as using multiple therapies with varying modes of action makes it more difficult for cancer cells to develop resistance.
However, combining tyrosine kinase inhibitors with other treatments is not without challenges. One of the main concerns is the potential for increased toxicity. Each therapy may have its own set of side effects, and combining them could lead to a higher risk of adverse events. Therefore, careful monitoring and dose adjustments may be necessary to manage these toxicities effectively.
Potential Combination Therapies Involving Tyrosine Kinase Inhibitors
| Treatment Modality | Indication | Combination Therapy |
|---|---|---|
| Chemotherapy | Lung Cancer | Tyrosine kinase inhibitor + Chemotherapy regimen (e.g., cisplatin and pemetrexed) |
| Immunotherapy | Melanoma | Tyrosine kinase inhibitor + Immune checkpoint inhibitor (e.g., pembrolizumab or nivolumab) |
| Hormonal Therapy | Breast Cancer | Tyrosine kinase inhibitor + Hormone receptor antagonist (e.g., tamoxifen or letrozole) |
In recent years, several clinical studies have investigated the efficacy and safety of combination therapies involving tyrosine kinase inhibitors. These studies have shown promising results, demonstrating improved response rates and prolonged progression-free survival in certain cancer types.
Overall, the field of combination therapy in cancer treatment is rapidly evolving. As researchers continue to explore different treatment combinations and optimize their regimens, the potential benefits of combining tyrosine kinase inhibitors with other therapies are becoming increasingly evident. With ongoing advancements in the understanding of cancer biology and treatment strategies, combination therapy holds great promise in improving outcomes for patients with tyrosine kinase-driven cancers.
Personalized Medicine and Tyrosine Kinase Cancer Treatment
Personalized medicine, also known as precision medicine, is revolutionizing the field of cancer treatment. It involves tailoring medical decisions and therapies to individual patients based on their unique genetic makeup, lifestyle, and environment. In the context of tyrosine kinase cancer treatment, personalized medicine plays a crucial role in improving patient outcomes.
Molecular profiling is at the forefront of personalized medicine in tyrosine kinase cancer treatment. By analyzing the genetic alterations and abnormalities that drive cancer development, molecular profiling helps oncologists identify specific tyrosine kinase targets and select appropriate targeted therapies. This approach allows for a more precise and effective treatment plan, minimizing unnecessary side effects and maximizing therapeutic benefits.
One of the key techniques used in molecular profiling is genetic testing, which involves analyzing a patient’s tumor DNA to identify specific genetic mutations or alterations. This information helps oncologists determine the most appropriate tyrosine kinase inhibitor for a particular patient. For example, in non-small cell lung cancer (NSCLC) patients with the EGFR mutation, tyrosine kinase inhibitors such as erlotinib (Tarceva) or osimertinib (Tagrisso) have shown remarkable success in improving survival rates and quality of life.
Besides genetic testing, other molecular profiling techniques such as RNA sequencing and proteomics can provide valuable insights into the complex molecular pathways involved in cancer development and progression. These techniques help identify additional targets for tyrosine kinase inhibitors and guide treatment decisions.
Benefits of Personalized Medicine in Tyrosine Kinase Cancer Treatment:
- Improved Treatment Efficacy: By targeting specific genetic alterations, personalized medicine enhances the effectiveness of tyrosine kinase inhibitors in fighting cancer cells. This approach increases response rates and improves patient outcomes.
- Reduced Side Effects: Tailoring treatment plans based on individual characteristics minimizes the likelihood of adverse reactions and unnecessary toxicity associated with non-targeted therapies.
- Optimized Treatment Selection: Molecular profiling enables oncologists to select the most appropriate tyrosine kinase inhibitor for each patient, increasing the chances of treatment success and avoiding ineffective therapies.
- Early Detection of Resistance: Personalized medicine facilitates the monitoring of treatment response and early detection of acquired or intrinsic resistance to tyrosine kinase inhibitors. This allows for prompt adjustment of treatment strategies and the exploration of alternative therapies.
Overall, personalized medicine holds great promise in tyrosine kinase cancer treatment. It allows for a tailored and more effective approach to combating cancer, improving patient outcomes, and offering hope for individuals facing this challenging disease.
Emerging Tyrosine Kinase Targets in Cancer
Continual advancements in cancer research have led to the identification of several emerging tyrosine kinase targets in various types of cancer. Understanding and targeting these specific kinases hold great promise in developing novel therapies for improved patient outcomes.
Tyrosine Kinase Targets
- ABL1: The ABL1 tyrosine kinase has been shown to play a crucial role in the development and progression of chronic myeloid leukemia (CML). Targeting ABL1 with tyrosine kinase inhibitors, such as imatinib, has revolutionized the treatment of CML and significantly improved patient survival rates.
- EGFR: Epidermal growth factor receptor (EGFR) is frequently mutated in non-small cell lung cancer (NSCLC) and has emerged as a promising therapeutic target. Tyrosine kinase inhibitors, such as erlotinib and gefitinib, have shown remarkable efficacy in NSCLC patients with EGFR mutations.
- HER2: HER2 gene amplification and overexpression are commonly observed in certain types of breast and gastric cancers. Targeted therapies, such as trastuzumab and lapatinib, which specifically inhibit HER2 tyrosine kinase activity, have significantly improved survival outcomes in HER2-positive cancer patients.
- FLT3: FMS-like tyrosine kinase 3 (FLT3) mutations are commonly found in acute myeloid leukemia (AML) and are associated with a poor prognosis. Inhibitors targeting FLT3, such as midostaurin and gilteritinib, have shown promising results in clinical trials, offering new treatment options for AML patients.
Novel Therapies and Clinical Trials
The identification of emerging tyrosine kinase targets has paved the way for the development of novel therapies. Ongoing clinical trials are investigating the efficacy of tyrosine kinase inhibitors against these targets in various cancer types, aiming to expand treatment options and improve patient outcomes.
Overcoming Challenges in Tyrosine Kinase Cancer Therapy
The use of tyrosine kinase inhibitors as a targeted therapy for cancer has shown remarkable results in improving patient outcomes. However, this approach is not without its challenges and limitations. In this section, we will explore the key challenges associated with tyrosine kinase cancer therapy and potential strategies to overcome them.
1. Drug Resistance
One of the major challenges in tyrosine kinase cancer therapy is the development of drug resistance. Cancer cells can acquire genetic alterations or activate alternative signaling pathways, rendering the tyrosine kinase inhibitors ineffective. This resistance can lead to disease progression and limited treatment options. Overcoming drug resistance is crucial for long-term treatment success.
2. Toxicity
Tyrosine kinase inhibitors can have side effects that impact patients’ quality of life. Common toxicities include fatigue, gastrointestinal disturbances, skin rash, and cardiovascular effects. Managing and minimizing toxicity is essential to ensure that patients can tolerate and adhere to their treatment regimen.
3. Lack of Biomarkers
Currently, there is a need for better diagnostic techniques and biomarkers to select patients who are most likely to benefit from tyrosine kinase inhibitors. Identifying predictive biomarkers can help personalize treatment decisions and improve patient outcomes. Research efforts are focused on identifying and validating reliable biomarkers for different tyrosine kinase inhibitors and cancer types.
4. Resistance to Combination Therapy
Combining tyrosine kinase inhibitors with other treatment modalities, such as chemotherapy or immunotherapy, holds promise for enhanced treatment response. However, resistance to combination therapy can still occur. Understanding the mechanisms underlying resistance to combination therapy is essential for optimizing treatment strategies and improving patient outcomes.
5. Patient Access and Affordability
Access to tyrosine kinase inhibitors can be a challenge for some patients due to their high cost and insurance coverage limitations. Ensuring broad accessibility and affordability of these targeted therapies is crucial to ensure that all patients who would benefit from them have the opportunity to receive effective treatment.
Despite these challenges, ongoing research and clinical trials are making strides in understanding and addressing these limitations. By overcoming these challenges, we can continue to improve the efficacy and safety of tyrosine kinase cancer therapy, ultimately benefiting patients worldwide.
| Challenges | Strategies |
|---|---|
| Drug Resistance | 1. Combination therapy 2. Novel targeted therapies |
| Toxicity | 1. Supportive care measures 2. Dose optimization |
| Lack of Biomarkers | 1. Molecular profiling 2. Biomarker discovery research |
| Resistance to Combination Therapy | 1. Mechanism-based approaches 2. Combinatorial strategies |
| Patient Access and Affordability | 1. Advocacy for policy changes 2. Development of generic options |
Tyrosine Kinase Cancer Clinical Trials
Tyrosine kinase inhibitors have revolutionized the field of cancer therapy by targeting specific proteins that drive tumor growth. As researchers continue to explore the potential of these inhibitors, numerous clinical trials are underway to evaluate their efficacy and safety in treating different types of cancer.
In recent years, tyrosine kinase inhibitors have shown promising results in improving patient outcomes, especially in cancers driven by specific genetic alterations. Clinical trials play a crucial role in assessing the effectiveness of these inhibitors, identifying optimal dosing regimens, and determining their potential role in combination therapies.
An ongoing clinical trial investigating the use of tyrosine kinase inhibitors in lung cancer has demonstrated impressive results. The study enrolled patients with non-small cell lung cancer (NSCLC) harboring specific mutations, such as EGFR or ALK alterations and evaluated the efficacy of targeted therapy. The results showed significantly improved progression-free survival and overall survival rates compared to standard chemotherapy.
Current Clinical Trials in Tyrosine Kinase Cancer Therapy
Table: Overview of Ongoing Tyrosine Kinase Cancer Clinical Trials
| Cancer Type | Trial Name | Targeted Protein | Treatment Arm | Phase |
|---|---|---|---|---|
| Chronic Myeloid Leukemia (CML) | IMATINIB1 | Bcr-Abl | Imatinib Mesylate | Phase III |
| Lung Cancer | OSIMERTINIB1 | EGFR | Osimertinib | Phase II |
| Colorectal Cancer | CETUXIMAB1 | EGFR | Cetuximab | Phase III |
These clinical trials not only provide valuable insights into the efficacy of tyrosine kinase inhibitors but also help identify potential biomarkers that can predict treatment response. By evaluating different patient populations, treatment combinations, and molecular markers, researchers are striving to develop more personalized and effective treatment strategies.
Moreover, clinical trials exploring novel tyrosine kinase inhibitors and combination therapies are continuously being developed to address the evolving challenges in cancer treatment. It is through these trials that advancements are made, ultimately leading to better outcomes for patients.
As the field of tyrosine kinase cancer therapy continues to progress, clinical trials will remain a crucial component in shaping the future of targeted treatment. By participating in these trials, patients not only gain access to potentially life-saving therapies but also contribute to the advancement of cancer research.
Side Effects of Tyrosine Kinase Inhibitors
Tyrosine kinase inhibitors (TKIs) are effective targeted therapies for various types of cancers. While TKIs have shown promising results in improving patient outcomes, they can also be associated with side effects. These side effects can vary depending on the specific TKI used and the individual patient’s response to the treatment.
Common side effects of tyrosine kinase inhibitors include:
- Fatigue: Many patients experience fatigue or a general feeling of tiredness while undergoing TKI treatment.
- Gastrointestinal issues: TKIs can cause nausea, vomiting, diarrhea, and loss of appetite in some patients.
- Rash and skin changes: Skin reactions, such as rash, dryness, or changes in skin color, are commonly reported side effects of TKIs.
- Cardiovascular effects: Some TKIs may impact the cardiovascular system, leading to hypertension (high blood pressure) or an increased risk of blood clotting.
- Hematological changes: TKIs can affect the production of blood cells, leading to anemia (low red blood cell count) or thrombocytopenia (low platelet count).
Managing Side Effects
It is crucial for healthcare providers to closely monitor patients receiving tyrosine kinase inhibitors to identify and manage any potential side effects. Various strategies can be employed to mitigate these side effects, including:
- Prescribing supportive medications to alleviate symptoms, such as anti-nausea medications for gastrointestinal issues.
- Advising patients to practice good skin care and providing recommendations for managing skin reactions.
- Monitoring cardiovascular health and addressing any cardiac-related concerns promptly.
- Regularly checking blood counts and adjusting treatment as needed to prevent severe hematological changes.
Patients need to communicate openly with their healthcare team about any side effects they experience to ensure timely intervention and appropriate management. By effectively managing side effects, healthcare providers can optimize the therapeutic benefits of tyrosine kinase inhibitors while improving patients’ quality of life during cancer treatment.
Future Directions in Tyrosine Kinase Cancer Research
As the field of tyrosine kinase cancer research continues to advance, several exciting future directions are emerging. These directions aim to further improve the efficacy and precision of targeted therapies, enhance our understanding of the underlying biology of tyrosine kinases, and develop novel treatment strategies for various types of cancers.
Development of New Targeted Therapies
One of the key future directions in tyrosine kinase cancer research involves the development of new targeted therapies. Scientists and researchers are actively exploring innovative ways to inhibit abnormal tyrosine kinase activity to disrupt cancer cell growth and survival. By identifying new tyrosine kinase targets and developing specific inhibitors, researchers hope to expand the range of treatment options available to patients.
Precision Oncology
Precision oncology, also known as personalized medicine, is an emerging field that aims to individualize cancer treatment based on the unique genetic alterations present in each patient’s tumor. In the future, tyrosine kinase cancer research is expected to play a significant role in precision oncology by identifying specific tyrosine kinase mutations and developing tailored treatment approaches for patients with these genetic alterations.
Advancements in Understanding Tyrosine Kinase Biology
Continued research efforts are focused on unraveling the complex biology of tyrosine kinases in cancer. By gaining a deeper understanding of the mechanisms by which these enzymes drive cancer growth and progression, researchers hope to identify vulnerabilities that can be exploited for therapeutic purposes. This knowledge will facilitate the development of more effective tyrosine kinase inhibitors and combination treatment strategies.
Exploration of Combination Therapies
Combining tyrosine kinase inhibitors with other treatment modalities, such as immunotherapy or chemotherapy, holds great promise for improving patient outcomes. Future directions in tyrosine kinase cancer research involve exploring the potential synergistic effects of these combination therapies and optimizing their use in different cancer types. Identifying the most effective treatment combinations, overcoming resistance mechanisms, and minimizing toxicity will be key areas of focus.
Advances in Diagnostic Techniques
Accurate and timely diagnosis is crucial for effective tyrosine kinase cancer treatment. Future research will likely focus on developing and refining diagnostic techniques that can quickly and reliably identify specific tyrosine kinase mutations. This will enable healthcare providers to tailor treatment plans and select the most appropriate tyrosine kinase inhibitors for individual patients, leading to improved outcomes and reduced treatment-related toxicity.
| Future Directions in Tyrosine Kinase Cancer Research |
|---|
| Development of new targeted therapies |
| Precision oncology and personalized medicine |
| Advancements in understanding tyrosine kinase biology |
| Exploration of combination therapies |
| Advances in diagnostic techniques |
Conclusion
In conclusion, the understanding of tyrosine kinase cancer targets has revolutionized the field of cancer treatment. Targeted therapy directed at inhibiting abnormal tyrosine kinase activity has emerged as a promising approach to combat various types of cancer. By specifically targeting the signaling pathways involved in cancer development, tyrosine kinase inhibitors have shown remarkable efficacy in slowing down the progression of the disease and improving patient outcomes.
The FDA-approved tyrosine kinase inhibitors have paved the way for personalized medicine in cancer treatment. Through molecular profiling, oncologists can identify specific genetic alterations in individual patients and tailor treatment plans accordingly. This approach ensures that patients receive the most effective treatment with minimal side effects.
Despite the significant progress made in the field, challenges such as drug resistance and toxicity still exist. Ongoing research aims to overcome these challenges by identifying new tyrosine kinase targets in various types of cancer. Additionally, the future direction of tyrosine kinase cancer research lies in the development of novel targeted therapies and the advancement of precision oncology.
In conclusion, tyrosine kinase cancer treatment has proven to be a valuable and promising approach in the fight against cancer. As research and clinical trials continue to explore new possibilities, it is clear that the identification and inhibition of tyrosine kinase cancer targets hold great potential in improving the lives of patients battling this devastating disease.
FAQ
What is tyrosine kinase?
Tyrosine kinase is an enzyme involved in cell signaling pathways that regulate important cellular processes. Abnormalities in tyrosine kinase activity can contribute to the development of cancer.
What role does tyrosine kinase play in cancer development?
Tyrosine kinase can drive uncontrolled cell growth, division, and survival, leading to the development and progression of cancer. Targeting tyrosine kinase activity has become a key strategy in cancer treatment.
What are the different types of cancers associated with abnormalities in tyrosine kinase activity?
Abnormalities in tyrosine kinase activity have been linked to various types of cancer, including chronic myeloid leukemia (CML), non-small cell lung cancer (NSCLC), and gastrointestinal stromal tumors (GIST), among others.
How do tyrosine kinase inhibitors work?
Tyrosine kinase inhibitors are drugs that suppress abnormal tyrosine kinase activity by blocking specific molecular targets. They work by interfering with the signaling pathways that promote cancer cell growth and survival.
Which tyrosine kinase inhibitors have been approved by the FDA?
The FDA has approved several tyrosine kinase inhibitors for the treatment of specific types of cancer, including imatinib (Gleevec) for CML, erlotinib (Tarceva) for NSCLC, and sunitinib (Sutent) for GIST, among others.
Can cancer patients develop resistance to tyrosine kinase inhibitors?
Yes, over time, cancer cells can develop resistance to tyrosine kinase inhibitors, leading to treatment failure. Various mechanisms contribute to the development of resistance, including genetic mutations and activation of alternative signaling pathways.
Are there any advantages to combining tyrosine kinase inhibitors with other treatments?
Combining tyrosine kinase inhibitors with other treatments, such as chemotherapy or immunotherapy, can enhance the effectiveness of therapy and improve patient outcomes. However, there may be challenges associated with drug interactions and increased toxicity.
How is personalized medicine used in tyrosine kinase cancer treatment?
Personalized medicine involves molecular profiling to identify specific genetic alterations in individual patients. This enables healthcare providers to tailor treatment plans using tyrosine kinase inhibitors that target the identified genetic abnormalities.
What are the latest advancements in identifying new tyrosine kinase targets in cancer?
Ongoing research is focused on identifying emerging tyrosine kinase targets in various types of cancer. This includes exploring potential novel therapies and conducting clinical trials to evaluate their efficacy and safety.
What are the challenges associated with tyrosine kinase cancer therapy?
Challenges in tyrosine kinase cancer therapy include the development of drug resistance, potential side effects of tyrosine kinase inhibitors, and the need for improved diagnostic techniques to identify patients who may benefit from targeted therapy.
What ongoing clinical trials are investigating tyrosine kinase inhibitors?
Numerous clinical trials are underway to evaluate the use of tyrosine kinase inhibitors in different types of cancer. These trials aim to uncover additional treatment options and advance the field of targeted therapy.
What are the common side effects of tyrosine kinase inhibitors?
Common side effects of tyrosine kinase inhibitors include fatigue, nausea, diarrhea, skin rashes, and high blood pressure. Healthcare providers need to monitor patients closely and manage these side effects.
What does the future hold for tyrosine kinase cancer research?
Future directions in tyrosine kinase cancer research include the development of new targeted therapies, advancements in precision oncology, and a deeper understanding of the underlying biology of tyrosine kinases in cancer.