Bile duct cancer stage 4 represents the most advanced form of this rare but aggressive disease. At this stage, the cancer has typically spread beyond the bile ducts to nearby organs, lymph nodes, or distant parts of the body such as the liver or lungs. Because of this progression, treatment becomes more complex and is primarily focused on extending life and improving quality of life rather than achieving a full cure.
Understanding bile duct cancer stage 4 is crucial for patients, families, and caregivers who are navigating the emotional and physical challenges that come with the diagnosis. This article explores in depth the causes, symptoms, diagnosis, treatment options, and the latest medical research that provides hope for better outcomes in the future.
Definition and Overview
Bile duct cancer, medically known as cholangiocarcinoma, is a malignancy that originates in the bile ducts — small tubes that carry bile from the liver and gallbladder to the small intestine. In stage 4 bile duct cancer, the cancer cells have metastasized, meaning they have spread beyond the bile ducts to distant organs. This stage is divided into:
- Stage 4A: Cancer has spread to nearby lymph nodes.
- Stage 4B: Cancer has spread to distant organs or tissues, such as the lungs, bones, or peritoneum.
Types of Bile Duct Cancer
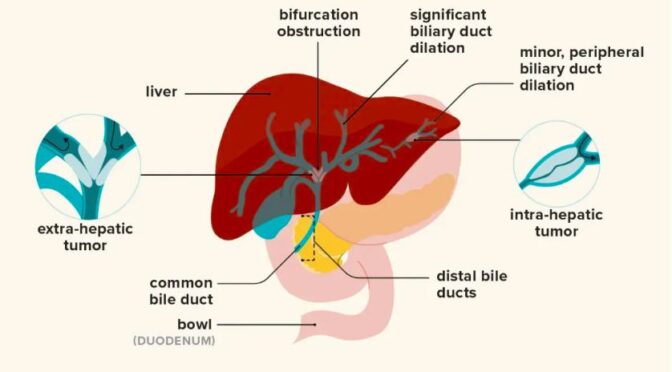
Bile duct cancer can occur in different locations along the bile duct system, and it is classified into three main types:
- Intrahepatic cholangiocarcinoma: Occurs inside the liver.
- Perihilar cholangiocarcinoma (Klatskin tumor): Occurs where the right and left hepatic ducts meet, just outside the liver.
- Distal cholangiocarcinoma: Occurs further down the bile duct, near the small intestine.
Each type presents unique challenges in terms of symptoms, treatment, and prognosis.
Causes and Risk Factors
While the exact cause of bile duct cancer is not fully understood, several risk factors increase the likelihood of developing it:
- Chronic bile duct inflammation (such as primary sclerosing cholangitis)
- Bile duct cysts or congenital abnormalities
- Chronic liver diseases, including cirrhosis and hepatitis B or C infection
- Gallstones or bile duct stones
- Exposure to toxins and certain industrial chemicals
- Older age and male gender
- Parasitic infections in the liver or bile ducts (common in some Asian countries)
Symptoms and Early Warning Signs
Symptoms of bile duct cancer stage 4 often develop gradually and may resemble other liver or gallbladder conditions. Common symptoms include:
- Persistent jaundice (yellowing of the skin and eyes)
- Abdominal pain, especially in the upper right quadrant
- Itchy skin and dark urine
- Pale or clay-colored stools
- Unintended weight loss and loss of appetite
- Fatigue and general weakness
- Fever or recurrent infections
In stage 4, symptoms may intensify due to metastasis, causing additional complications such as fluid buildup (ascites), bone pain, or breathing difficulties.
Diagnosis
Diagnosing bile duct cancer stage 4 involves multiple tests and imaging studies to determine the extent of cancer spread. Common diagnostic tools include:
- Blood tests: To check liver function and tumor markers such as CA 19-9.
- Imaging tests: Ultrasound, CT scan, MRI, or PET scan to visualize tumors.
- Biopsy: Tissue sample analysis confirms cancer presence and type.
- Endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic cholangiography (PTC): Specialized procedures to visualize the bile ducts and collect tissue samples.
Treatment Options
Treatment for stage 4 bile duct cancer focuses on managing symptoms, slowing disease progression, and improving quality of life. Common approaches include:
- Chemotherapy: Drugs such as gemcitabine and cisplatin are standard first-line treatments.
- Targeted therapy: For patients with specific genetic mutations (e.g., FGFR2 or IDH1), targeted drugs like pemigatinib may be used.
- Immunotherapy: Drugs such as pembrolizumab can help the immune system attack cancer cells.
- Radiation therapy: Used to relieve pain and control tumor growth.
- Biliary drainage or stenting: Helps relieve jaundice and improve bile flow.
- Palliative care: Focuses on symptom management and emotional support for patients and families.
Prevention and Lifestyle Recommendations
While not all cases can be prevented, several lifestyle adjustments can help reduce the risk of bile duct cancer:
- Avoid chronic liver infections by getting vaccinated for hepatitis B and practicing safe hygiene.
- Limit alcohol consumption and maintain a healthy weight to reduce liver strain.
- Avoid exposure to toxic chemicals and industrial pollutants.
- Regular medical check-ups if you have a history of liver or bile duct disease.
- Eat a balanced diet rich in fruits, vegetables, and whole grains to support liver health.
Prognosis and Survival Rates
The prognosis for bile duct cancer stage 4 is generally poor, as the disease is often diagnosed at an advanced stage. The five-year survival rate is typically less than 10%, depending on the cancer’s location, response to treatment, and overall health of the patient. However, recent advancements in targeted therapy and immunotherapy have improved outcomes for some patients, offering extended survival and better quality of life.
Latest Research and Innovations
Recent studies are uncovering promising treatment approaches for bile duct cancer stage 4, including:
- Next-generation sequencing (NGS): Helps identify genetic mutations for personalized treatment.
- Immunotherapy combinations: Trials exploring the use of immunotherapy alongside chemotherapy.
- Nanotechnology-based drug delivery: Enhancing the precision and effectiveness of chemotherapy drugs.
- Liver transplantation research: In select cases, transplant may be considered following successful tumor control.
These innovations are bringing renewed hope to patients and pushing the boundaries of what’s possible in bile duct cancer care.
Coping and Support for Patients
A stage 4 bile duct cancer diagnosis can be emotionally and physically overwhelming. Patients are encouraged to:
- Seek psychological counseling or join support groups.
- Work with a multidisciplinary care team including oncologists, nutritionists, and palliative care specialists.
- Engage in gentle physical activity and maintain a supportive social network.
- Consider integrative therapies such as mindfulness, meditation, or yoga to manage stress and improve well-being.
Conclusion
While bile duct cancer stage 4 remains a serious and challenging condition, medical advances continue to improve treatment options and survival rates. Early detection, personalized therapy, and comprehensive support can make a significant difference in the patient’s journey. Awareness, research, and compassionate care remain key to improving outcomes and providing hope to those affected by this rare cancer.
Frequently Asked Questions (FAQ)
1. Is bile duct cancer stage 4 curable?
No, it is not considered curable at this stage, but treatment can help control symptoms and extend survival.
2. How long can someone live with stage 4 bile duct cancer?
Life expectancy varies but typically ranges from 6 months to 2 years, depending on response to treatment and overall health.
3. Can surgery be done for stage 4 bile duct cancer?
Surgery is usually not an option since the cancer has spread, but procedures to relieve bile duct blockage may be performed.
4. What are the latest treatments for bile duct cancer stage 4?
Targeted therapy, immunotherapy, and clinical trials exploring personalized medicine offer new possibilities for treatment.
5. How can patients improve their quality of life during treatment?
Maintaining a healthy diet, engaging in light exercise, managing pain effectively, and seeking emotional support are vital for quality of life.