Stagescancer.net – Among the varied and complex malignancies afflicting the lymphatic system, mesenteric lymph node cancer stands out as a particularly rare and challenging type of abdominal lymphoma. This form of rare lymphatic cancer presents a unique set of difficulties, compelling both patients and healthcare professionals to seek a deeper understanding of its nuances. Little known outside specialist circles, these lymphatic system malignancies necessitate heightened awareness to improve diagnostic procedures and therapeutic outcomes.
Overview of Mesenteric Lymphoma
Mesenteric lymphoma, a subset of non-Hodgkin lymphoma (NHL), specifically targets the gastrointestinal tract, leading to a unique set of challenges in its identification and management. This cancer is characterized by the clonal proliferation of lymphocytes within the mesentery, the fold of tissue attaching the intestines to the abdominal wall. Due to the diversity of lymphoma types, an in-depth cancer overview including both B-cell and T-cell lymphomas is crucial, as these subtypes dictate the course of the disease, influence clinical presentations, and necessitate specialized treatment approaches. As abdominal cancers, such as mesenteric tumors, can often be elusive, raising awareness among healthcare professionals and patients is pivotal for enhancing earlier detection rates and thereby potentially improving patient outcomes.
| Lymphoma Classification | Primary Location | Distinguishing Features | Common Treatment Approaches |
|---|---|---|---|
| B-cell Lymphomas | Mesentery | Abnormal B-lymphocyte proliferation | Chemotherapy, Immunotherapy |
| T-cell Lymphomas | Mesentery and Surrounding Tissue | Clonal T-lymphocyte malignancy | Targeted Therapy, Stem Cell Transplant |
The advancement in the understanding of mesenteric lymphoma is an ongoing quest within oncology, with continuous research efforts geared toward refining diagnostic techniques and treatment modalities. These endeavors leverage the intricate knowledge we have about the histological landscape of abdominal cancers, enabling us to steadily improve the quality of life and prognoses for patients grappling with these challenging mesenteric tumors.
Signs and Symptoms of Mesenteric Lymphoma
Recognizing the early signs and symptoms of mesenteric lymphoma can be challenging due to their non-specific nature. Understanding these manifestations is crucial for prompt diagnosis and effective treatment. Commonly reported indicators include persistent abdominal discomfort, noticeable weight loss, and various gastrointestinal complications, which may mimic other less serious conditions.
Abdominal Pain and Swelling
Many patients experience a combination of abdominal pain and swelling as initial lymphoma symptoms. This discomfort can range from mild to severe and may be accompanied by a bloated feeling or a noticeable increase in abdominal girth. Such symptoms are not only distressing but also vague in their presentation, which can delay the diagnosis of underlying lymphatic system malignancies.
Unintended Weight Loss
A concerning symptom that often accompanies mesenteric lymphoma is unintended weight loss. It is a red flag for many health professionals as it indicates a possibility of advanced disease. Weight loss in patients with cancer could be due to a combination of factors including decreased appetite, malabsorption, and increased metabolic demand by the tumor.
Gastrointestinal Symptoms
Patients with mesenteric lymphoma may also suffer from a range of gastrointestinal symptoms. These can include nausea, vomiting, diarrhea or constipation, and changes in bowel habits. These gastrointestinal disturbances highlight the complexities of the disease and underscore the importance of considering lymphoma in the differential diagnosis of such symptoms.
Diagnosis of Mesenteric Lymphoma
The journey to an accurate cancer diagnosis begins with a combination of sophisticated lymphoma imaging tests and meticulous biopsy analysis. These diagnostic tools are fundamental in identifying and classifying mesenteric lymphoma, ultimately leading to a refined treatment plan tailored to the pathology of the lymph nodes.
The Essential Role of Imaging in Diagnoses
Medical imaging serves as the first line of sight in detecting anomalies within the lymphatic system. Technologies such as computed tomography (CT) scans and magnetic resonance imaging (MRI) are instrumental in visualizing the extent and location of lymph node involvement. Through detailed images, radiologists can assess the size, shape, and consistency of mesenteric lymph nodes, paving the way for a more targeted approach in subsequent biopsies.
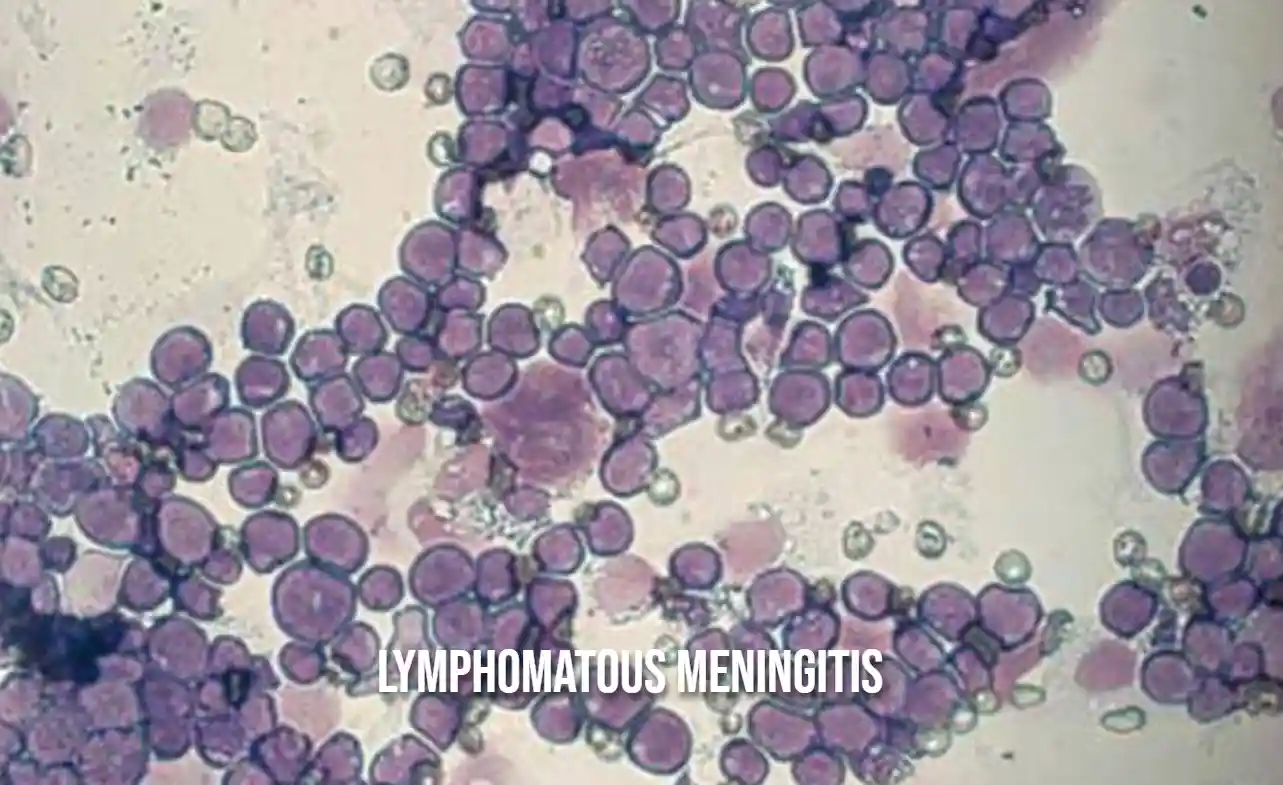
Biopsy Procedures and Pathology
Following imaging, a biopsy is crucial for establishing a definitive diagnosis. Pathologists perform thorough biopsy analysis on extracted tissue samples, assessing the cellular makeup and identifying malignancy. Advanced techniques such as immunophenotyping and genetic profiling further classify the lymphoma subtype, providing insight into the behavior of the cancer and informing prognosis. This pathology-driven verification process ensures that the complexities of mesenteric lymphoma are understood before commencing treatment.
- Utilization of CT and MRI scans to detect lymphoma presence and extent
- Application of fine-needle aspiration or core needle biopsy to obtain tissue samples
- Detailed pathological examination including immunohistochemistry and molecular studies for subtype identification
Pathophysiology of Mesenteric Lymphoma
The intricate details of cancer pathophysiology are essential to comprehending mesenteric lymphoma. As a lymphatic system disease, this malignancy disrupts the mesenteric lymph node function, which is vital for maintaining the body’s immune defenses. By mapping the tumor growth patterns, one can gain insight into this aggressive disease’s origin and progression.
Mesenteric lymphoma primarily involves abnormal proliferation of either B-cells or T-cells within the lymphatic tissue of the mesentery. This abnormal growth leads to progressive interference with the lymphatic system’s natural operations. Normal lymph node architecture is compromised, eroding the nodes’ capacity to filter bodily fluids and fight infections effectively. The mesenteric lymph nodes, located in the abdomen, thus become sites for uncontrolled cancerous growths.
Disruption of these lymphatic functions manifests in several clinical ways. Patients often experience systemic symptoms such as weight loss and fatigue, as well as abdominal-specific distress including pain and bloating. To encapsulate the disease’s complexity, the following table summarizes the key components of mesenteric lymphoma’s pathophysiology:
| Component | Description | Effect on Lymphatic Function |
|---|---|---|
| Cell Origin | B-cells or T-cells malignancy within mesentery | Monoclonal lymphocyte proliferation disrupting lymph node structure |
| Node Architecture | Disrupted by tumor growth | Impaired filtration and immune response |
| Growth Patterns | Can be localized or diffuse, affecting one or more lymph nodes | Varying degrees of systemic impact and symptom presentation |
Understanding these aspects is not just academically significant; it is a cornerstone in devising effective therapeutic strategies to combat mesenteric lymphoma.
Staging and Prognosis of Mesenteric Lymphoma
The process of cancer staging is critical in mesenteric lymphoma due to its direct correlation with treatment decisions and lymphoma prognosis. Staging encompasses evaluating the extent of disease progression, including the size and spread of tumors as well as their presence in other parts of the body. This information is essential for clinicians to forecast survival rates and plan an effective course of action.
Understanding Mesenteric Lymphoma Stages
Stages of mesenteric lymphoma categorize the severity of the disease from early, localized stages to advanced, widespread involvement. These stages guide oncologists in determining the most effective treatment protocols.
Factors Influencing Prognosis
Several key factors are taken into consideration when predicting an individual’s prognosis with mesenteric lymphoma. These factors include:
- Age of the patient at diagnosis
- Size and number of lymph nodes affected
- The histological subtype of the lymphoma
- The patient’s response to initial therapy
Typically, younger patients with smaller tumors that respond well to treatment have a more favorable prognosis. Conversely, advanced stages with large tumor burden are associated with a poorer prognosis and may require more aggressive treatment strategies to manage the disease effectively.
Treatment Options for Mesenteric Lymphoma
The management of mesenteric lymphoma involves a multi-faceted approach, often requiring the integration of various cancer treatments to address this complex malignancy. Developing an effective treatment regimen takes into account the specific subtype of lymphoma, its stage, and the overall health of the patient. Let us delve into the primary treatment methodologies employed in battling this rare form of cancer.
Chemotherapy and Targeted Therapy
Chemotherapy regimens serve as a cornerstone in the treatment of mesenteric lymphoma, with protocols designed to target rapidly dividing lymphoma cells. These systemic therapies are often combined with targeted drugs that pinpoint unique markers on cancer cells, thereby reducing collateral damage to healthy tissue and enhancing treatment efficacy. The precision of targeted therapy represents a significant advancement in cancer treatment modality, aiming to improve patient outcomes and minimize adverse effects.
Radiation Treatment
For cases where mesenteric lymphoma is localized or when symptom management is at the forefront, radiation therapy offers a targeted approach to reducing tumor burden. This form of treatment employs high-energy rays to destroy cancer cells, providing relief from pain and other symptoms caused by tumor growth. Radiation therapy continues to evolve, with techniques becoming increasingly refined to deliver maximum therapeutic benefit while sparing surrounding healthy tissues.
The Role of Surgery in Treatment
While surgical oncology is not typically the mainstay of mesenteric lymphoma management, surgical intervention is indeed crucial in certain contexts. Surgically removing sections of the tumor can aid in relieving intestinal blockages or extracting tissue for a definitive diagnosis. These procedures are essential for maintaining quality of life and for the accurate staging of the disease, which in turn informs the subsequent steps in the treatment plan.
Role of Diet and Nutrition in Managing Mesenteric Lymphoma
Adequate lymphoma nutrition and cancer diet considerations are indispensable elements in the comprehensive care of patients battling mesenteric lymphoma. The inclusion of personalized nutritional support strategies not only sustains physical health but may also improve treatment efficacy and patient quality of life. Dietary management during the cancer journey is not only about meeting basic nutritional needs; it is about strategically tailoring food choices to enhance the patient’s overall well-being and to combat the multifaceted challenges presented by the disease and its treatment.
- Maintaining Muscle Mass and Weight: High-calorie, high-protein diets may help patients prevent muscle wasting and maintain a healthy weight.
- Managing Symptoms and Side Effects: Nutritional adjustments can be made to alleviate common symptoms such as nausea, loss of appetite, and digestive issues.
- Supporting Immune Function: A diet rich in antioxidants, vitamins, and minerals supports the immune system during and after treatment.
- Promoting Healing and Recovery: Adequate nutrition is crucial for recovery, especially after surgical interventions or during chemotherapy and radiation therapy cycles.
It is recommended that a certified dietitian be involved in the care team for mesenteric lymphoma patients to offer targeted nutritional support tailored to each individual’s requirements. The dietitian can assess the patient’s nutritional status, recommend appropriate dietary modifications, and monitor progress throughout treatment and into survivorship.
Psychological Impact of Mesenteric Lymphoma
The journey through a rare cancer diagnosis, such as mesenteric lymphoma, is fraught with not only physical challenges but also profound mental health in cancer care considerations. The onset of this disease marks the beginning of a multifaceted battle, in which cancer psychology plays a critical role. Studies demonstrate that a significant number of patients grappling with lymphoma confront heightened levels of anxiety and depression, which can exacerbate the physical symptoms of the illness and affect overall patient well-being.
Given the intricate interplay between the mind and body, acknowledging and addressing the lymphoma’s emotional effects is paramount in the comprehensive care of patients. The impact on mental health poses a peculiar challenge for healthcare providers, as the psychological ramifications of mesenteric lymphoma can manifest in a spectrum of ways, from subtle mood changes to profound psychological distress.
Here is a synopsis of key emotional states often encountered by mesenteric lymphoma patients, and strategies for support:
- Anxiety due to uncertain prognosis and treatment outcomes
- Depression stemming from the disease burden and treatment side effects
- Sense of isolation as a result of rare cancer diagnosis and potential lack of support networks
Integrated care teams, particularly mental health professionals, are therefore indispensable in providing ongoing emotional and psychological support. Such support often includes, but is not limited to, counseling services, anxiety management strategies, and depression treatment, which together serve to buttress a patient’s psychological resilience throughout their cancer journey.
| Emotional State | Effects on Patients | Support Strategies |
|---|---|---|
| Anxiety | Fear, sleep disturbances, difficulty concentrating | Counseling, medication, stress-relief techniques |
| Depression | Chronic sadness, withdrawal, change in appetite | Psychotherapy, support groups, antidepressants |
| Isolation | Loneliness, decreased social interaction | Peer support networks, family counseling, community programs |
It is incumbent upon medical teams to recognize that the journey with mesenteric lymphoma does not solely revolve around physical treatment; it also necessitates a judicious approach to maintaining patient well-being. Balancing the clinical treatment with emotional care enables a holistic approach, which is proving increasingly vital in the realm of cancer recovery and quality of life.
Current Research on Mesenteric Lymphoma
The landscape of lymphoma research is ever-evolving, with scientific advancements opening new paths for cancer therapeutic development. In the relentless pursuit of conquering mesenteric lymphoma, researchers and clinicians worldwide are dedicated to unraveling the intricacies of this disease to formulate novel treatments and enhance patient care.
Advancements in Treatment
Recent breakthroughs in treatment options mark a significant milestone in mesenteric lymphoma care. With a specific emphasis on improving the targeted delivery of drugs, the focus has been on optimizing efficacy while minimizing adverse effects. This precision medicine approach is reflective of a broader trend in oncology towards personalized healthcare.
Clinical Trials and Emerging Therapies
Central to the progress in mesenteric lymphoma therapy are ongoing clinical studies that seek to determine the potential of various emerging therapies. These studies are vital in ascertaining the safety and effectiveness of new treatment regimens, which may include combinations of immunotherapy, targeted drugs, and other novel therapeutic strategies. The collective efforts of these research initiatives bear the promise of advancing patient outcomes and ushering in a new era of treatment possibilities.
Mesenteric Lymphoma Case Studies
Exploring lymphoma case studies sheds light on the intricacies of patient experiences, from initial symptoms to long-term treatment outcomes. These reports are pivotal in understanding both the successes and the oncology challenges faced in treating this rare form of cancer. By delving into patient case reports, we gain invaluable insights that contribute to the advancement of therapeutic strategies and patient care in oncology.
Real-Life Treatment Success Stories
Success stories in the treatment of mesenteric lymphoma offer a beacon of hope and provide vital learning opportunities. They highlight the effects of personalized treatment plans and the importance of early intervention. Moreover, they underscore the advancements in medicine that have contributed to improving patient survival and quality of life.
-
- Case Study 1:
A patient diagnosed at an early stage who achieved full remission with an innovative chemotherapy regimen.
-
- Case Study 2:
An individual who was part of a clinical trial for a targeted therapy resulted in significant tumor shrinkage and improved outcomes.
-
- Case Study 3:
A story of a patient managing the disease with a combination of radiation and immunotherapy, highlighting the promise of multimodal treatments.
Challenges in Treating Mesenteric Lymphoma
Oncology professionals continually confront hurdles as they strive to tackle mesenteric lymphoma effectively. Each case brings unique challenges, from managing side effects to navigating the emotional toll of cancer treatment. These challenges draw attention to the need for ongoing research and development in the field.
| Challenge | Description | Impact on Treatment |
|---|---|---|
| Late Diagnosis | Non-specific symptoms lead to the late discovery of the disease. | Decreases treatment effectiveness and chances of remission. |
| Treatment Resistance | The patient’s disease does not respond to standard therapy protocols. | Requires the exploration of alternative or experimental treatments. |
| Recurrence | The patient experiences relapse after achieving initial remission. | Necessitates a revised treatment approach, often more aggressive and with greater risk of side effects. |
Support Systems and Resources for Patients
For individuals diagnosed with mesenteric lymphoma, finding comprehensive lymphoma patient support and dependable healthcare resources is crucial for managing the disease effectively. Engaging with support networks can provide not only social and emotional bolstering but also education on managing lymphoma and patient advocacy. Access to these support avenues is essential to forge a solid foundation for treatment and recovery.
Peer Support and Online Communities
Peer support groups and online support networks play a pivotal role in a patient’s journey. These platforms allow individuals to connect with others who understand the complexities of living with lymphoma. Online support networks can break the barriers of geographical isolation, offering a haven for sharing experiences, advice, and encouragement from peers and healthcare professionals alike.
Navigating Healthcare Services
Navigating through the maze of healthcare services can be overwhelming for lymphoma patients and their families. Recognizing this challenge, patient advocacy groups and healthcare resources are invaluable guides, ensuring patients access the necessary treatments and support. These services also provide information on insurance, rights, and clinical trials, which can be critical to receiving high-quality care and financial assistance.
- Local and National Cancer Support Organizations
- Online Forums and Social Media Groups
- Advocacy and Guidance on Healthcare Navigation
- Educational Resources and Literature
- Virtual Counseling and Mental Health Services
| Resource | Type of Support | Availability |
|---|---|---|
| Cancer Support Community | Emotional, Educational | 24/7 Online, Local Chapters |
| Lymphoma Research Foundation | Research, Advocacy | Business Hours, Online Resources |
| The Leukemia & Lymphoma Society | Financial Support, Advocacy | Business Hours, Online Resources |
| American Cancer Society | Educational, Support Programs | 24/7 Call Center, Online |
| National Coalition for Cancer Survivorship | Advocacy, Education | Business Hours, Online Resources |
Complications and Relapse in Mesenteric Lymphoma
Among individuals diagnosed with mesenteric lymphoma, lymphoma complications are not uncommon. These complications are multifaceted, ranging from infections and organ dysfunction to bowel obstructions that may necessitate acute medical interventions. Due to the lymphoma’s location in the abdomen, these complications can severely impact a patient’s digestive processes and overall quality of life.
Moreover, cancer recurrence or relapse introduces added layers of complexity to treatment and survivorship plans. Managing a mesenteric lymphoma relapse requires a nuanced approach, considering variables such as the nature of the initial treatment, the biological behavior of the cancer, and the individual’s current health status. This diligence aims to effectively target the cancer and uphold the patient’s quality of life.
- Infections – a common complication due to the compromised immune system of lymphoma patients.
- Bowel Obstruction – resulting from tumor growth or due to the aftereffects of treatments like surgery or radiation.
- Organ Dysfunction – lymphatic infiltration and treatment toxicity can impair organ function.
Addressing long-term cancer effects entails ongoing surveillance and supportive care. Medical teams must be vigilant in monitoring for any signs of relapse, which often involves imaging studies and routine clinical assessments. In addition to medical interventions, adopting comprehensive lifestyle changes such as nutrition optimization and stress management techniques may aid in mitigating long-term adverse effects.
When it comes to managing relapse, a personalized strategy is adopted depending on the relapse’s timing, location, and the patient’s prior treatment regimen. Such a strategy often involves novel therapeutic agents or protocols that were not part of the initial treatment course. Engaging with a multispecialty team facilitates a robust plan of action should relapse occur, underscoring the dynamic field of oncology and its commitment to life-enhancing solutions for patients battling mesenteric lymphoma.
- Diligent follow-up appointments to monitor for signs of relapse.
- Application of multimodal therapies possibly including new clinical trial options tailored to relapse specifics.
- Focus on symptom management and palliative care to maintain the patient’s quality of life.
Overall, a comprehensive treatment plan that involves regular monitoring, prompt management of complications, and adaptive strategies for relapse can significantly contribute to improving outcomes for patients with mesenteric lymphoma.
Mesenteric Lymphoma Survival Rates and Statistics
Delving into the survival statistics of mesenteric lymphoma, it is essential to acknowledge the variability that exists based on several key factors. The stage at which the cancer is diagnosed plays a significant role in the survival prognosis, with early detection generally associated with better outcomes. However, it’s not just the timing of the diagnosis that influences this; the histological subtype of the lymphoma and the patient’s overall health condition are also critical components. These components are intricately linked to oncology epidemiology and influence the development of targeted treatment protocols aimed at extending survival and improving the quality of life for affected individuals.
Epidemiological data concerning mesenteric lymphoma are critical; they provide insights that can lead to improvements in patient management and treatment effectiveness. Understanding the trends over time, including increases or decreases in survival rates, allows healthcare professionals to gauge the impact of new therapies and adjust patient care strategies accordingly. Gathering cancer survival rates across different demographics and regions can also shed light on potential socioeconomic and environmental factors affecting disease prevalence and outcomes.
The importance of meticulous data collection and rigorous analysis cannot be overstated in the realm of cancer care, where every insight can lead to a life-saving breakthrough. For mesenteric lymphoma, ongoing research and persistent examination of disease patterns are fundamental to elevating the standard of care. It is through the relentless pursuit of knowledge in this field that the medical community strives to offer a beacon of hope for those navigating the challenges of this rare yet formidable cancer.
FAQ
What exactly is mesenteric lymphoma?
Mesenteric lymphoma is a rare type of cancer that affects the lymphatic system, specifically the lymph nodes in the mesentery, a fold of tissue in the abdomen. It is a form of non-Hodgkin lymphoma that relates to lymphatic system malignancies and presents challenges in diagnosis and treatment.
What are the symptoms of mesenteric lymphoma?
Symptoms can include non-specific indicators such as abdominal pain and swelling, unintended weight loss, and various gastrointestinal symptoms like nausea, vomiting, and changes in bowel habits. The presentation of symptoms often makes initial diagnosis difficult.
How is mesenteric lymphoma diagnosed?
Diagnosis typically involves imaging tests like CT scans and MRIs to identify abnormalities in the mesenteric lymph nodes. A biopsy is then done to provide pathological confirmation, and further tests such as immunophenotyping and genetic studies can help with subtype classification.
Are there different types of mesenteric lymphoma?
Yes, mesenteric lymphoma can have varied histological subtypes, including B-cell and T-cell lymphomas, each dictating different clinical presentations and treatment approaches.
What treatment options are available for mesenteric lymphoma?
Treatment strategies are individualized and may include chemotherapy and targeted therapies suited to specific lymphoma subtypes, radiation therapy for localized disease or symptom relief, and sometimes surgery for obstructions or other complications.
What is the prognosis for someone with mesenteric lymphoma?
The prognosis for mesenteric lymphoma varies depending on factors such as the stage of the disease, age of the patient, tumor size and subtype, and response to therapy. Advanced stages are typically associated with a poorer prognosis, though ongoing research and treatment advancements continually improve outcomes.
How does diet and nutrition impact the management of mesenteric lymphoma?
Proper nutrition plays a supportive role in managing mesenteric lymphoma, as it can help maintain strength, body weight, and overall well-being. Dietary adjustments may be necessary to manage symptoms and side effects of treatments. Collaborating with a dietitian for specialized dietary plans is often recommended.
What are the emotional effects of mesenteric lymphoma on patients?
Being diagnosed with a rare cancer such as mesenteric lymphoma can cause significant emotional and psychological distress. Patients may face anxiety, depression, and feelings of isolation. It is crucial to provide mental health support and counseling to help manage these challenges.
What are some current advancements in mesenteric lymphoma research?
Researchers are actively working on improving treatments through the development of novel drugs, targeted therapies, and immunotherapy approaches. Clinical trials are essential for testing new treatment protocols and combinations to enhance patient survival and quality of life.
Where can patients with mesenteric lymphoma find support?
Patients can access a variety of support systems, including peer support groups, online communities, and patient advocacy organizations. These networks provide emotional support, educational resources, and assistance in navigating healthcare services, all of which can be instrumental in a patient’s cancer journey.
Can mesenteric lymphoma recur, and how are complications managed?
Yes, mesenteric lymphoma can recur, and complications from the disease or treatment may include infections, bowel obstruction, and organ dysfunction. Management of a relapse depends on prior treatments and the patient’s overall health. Continuous monitoring and swift intervention are critical for managing complications effectively.
What survival rates and statistics are available for mesenteric lymphoma?
Survival rates for mesenteric lymphoma depend on various factors, including the disease’s stage at the time of diagnosis, the histological subtype, and specific patient characteristics. Ongoing collection and analysis of epidemiological data are important for understanding the disease better and improving evidence-based care.