Hemoptysis, or coughing up blood, is one of the most alarming symptoms a person can experience, especially when linked to lung cancer. This condition often signals advanced respiratory issues and requires immediate medical attention. While not every case of hemoptysis is caused by cancer, the association between hemoptysis and lung cancer makes it a crucial warning sign that should never be ignored.
Understanding hemoptysis in the context of lung cancer can help patients, families, and healthcare providers identify early warning signs, seek prompt treatment, and improve outcomes. In this article, we will explore the definition, causes, risk factors, diagnosis, treatment options, prevention strategies, prognosis, and the latest research on hemoptysis in lung cancer.
Definition and Overview
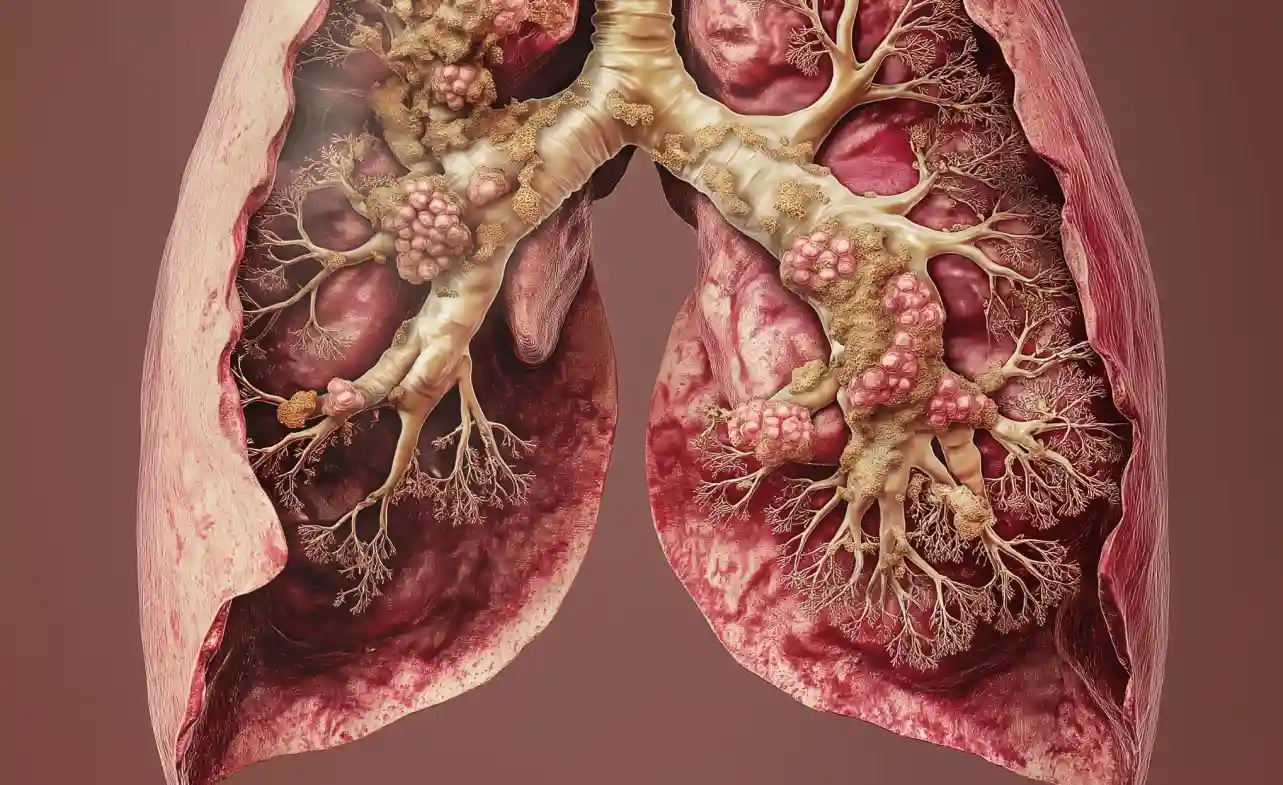
Hemoptysis refers to the expectoration of blood from the lower respiratory tract, usually through coughing. In patients with lung cancer, hemoptysis occurs when tumors invade blood vessels within the lungs, leading to bleeding. While minor cases may involve streaks of blood in sputum, severe cases can result in life-threatening hemorrhage.
In the context of lung cancer, hemoptysis is both a symptom and a clinical challenge. It is estimated that 20–50% of lung cancer patients experience hemoptysis at some stage of their disease, making it a significant clinical concern for oncologists and pulmonologists worldwide.
Types of Hemoptysis in Lung Cancer
Hemoptysis is generally classified based on severity:
- Mild Hemoptysis – Small amounts of blood-streaked sputum.
- Moderate Hemoptysis – Noticeable but non-life-threatening bleeding.
- Massive Hemoptysis – Life-threatening bleeding, often exceeding 200–600 mL in 24 hours, requiring urgent intervention.
Recognizing the type of hemoptysis is vital for determining treatment urgency and managing complications effectively.
Causes and Risk Factors
In lung cancer patients, hemoptysis commonly occurs due to:
- Tumor invasion of bronchial blood vessels
- Inflammation and infection around tumors
- Post-radiation or chemotherapy complications
- Blood clotting abnormalities in advanced cancer
Risk factors that increase the likelihood of hemoptysis in lung cancer include:
- Smoking history (primary risk factor for lung cancer)
- Chronic lung diseases such as COPD or tuberculosis
- Genetic predisposition
- Occupational exposure to asbestos, radon, or other carcinogens
Symptoms and Early Warning Signs
Alongside hemoptysis, other lung cancer symptoms may include:
- Persistent cough that worsens over time
- Chest pain or discomfort
- Shortness of breath
- Unexplained weight loss
- Fatigue and weakness
- Hoarseness or wheezing
Early recognition of these warning signs, especially when combined with hemoptysis, can significantly improve diagnostic and treatment outcomes.
Diagnosis
Diagnosing hemoptysis in lung cancer involves multiple steps:
- Medical history and physical examination
- Chest X-ray to detect abnormalities
- CT scan for detailed imaging of lung structures
- Bronchoscopy to visualize and identify bleeding sites
- Sputum cytology to detect malignant cells
- Biopsy for confirming cancer diagnosis
Accurate diagnosis helps distinguish hemoptysis due to lung cancer from other causes such as infections, bronchiectasis, or pulmonary embolism.
Treatment Options
Treatment of hemoptysis in lung cancer focuses on controlling bleeding and managing the underlying cancer. Common approaches include:
- Bronchial artery embolization (BAE) – Minimally invasive procedure to stop bleeding.
- Endobronchial therapies – Laser therapy, cryotherapy, or stent placement.
- Surgical intervention – Lobectomy or pneumonectomy in selected cases.
- Oncological treatment – Chemotherapy, radiotherapy, targeted therapy, and immunotherapy.
Treatment is highly individualized based on the severity of hemoptysis, cancer stage, and patient health condition.
Prevention and Lifestyle Recommendations
Although not all cases of hemoptysis in lung cancer can be prevented, lifestyle changes and proactive health management reduce risks:
- Quitting smoking and avoiding secondhand smoke
- Regular medical check-ups for high-risk individuals
- Healthy diet rich in antioxidants
- Regular physical activity to maintain lung health
- Avoiding occupational exposure to carcinogens
Prognosis and Survival Rates
The prognosis for patients with hemoptysis due to lung cancer depends on several factors:
- Cancer stage at diagnosis
- Type of lung cancer (small cell vs. non-small cell)
- Patient’s overall health and comorbidities
- Response to treatment
Generally, massive hemoptysis is associated with poor outcomes. However, early detection and advanced therapies have significantly improved survival rates in recent years.
Global Impact
Lung cancer with hemoptysis is a global health concern, ranking as one of the leading causes of cancer-related deaths worldwide. Developing countries face additional challenges due to delayed diagnosis, limited access to healthcare, and high smoking prevalence. Raising awareness about hemoptysis as a symptom can promote earlier detection and intervention globally.
Latest Research and Innovations
Recent innovations in managing hemoptysis in lung cancer include:
- Targeted therapies that attack specific cancer cells
- Immunotherapy to boost the body’s immune response
- Robotic-assisted surgery for precision tumor removal
- Advanced embolization techniques for safer and more effective bleeding control
Ongoing clinical trials are exploring novel drugs and minimally invasive procedures aimed at improving patient survival and quality of life.
Coping and Support for Patients
Experiencing hemoptysis with lung cancer can be physically and emotionally overwhelming. Patients benefit from:
- Psychological counseling and support groups
- Palliative care for pain and symptom management
- Family and caregiver education
- Nutritional support to strengthen the immune system
- Access to community and online support resources
Holistic care ensures patients and their families maintain hope and resilience throughout treatment.
Conclusion
Hemoptysis in lung cancer is a critical clinical symptom that requires urgent medical evaluation and intervention. While it poses serious challenges, advancements in diagnosis and treatment provide patients with better chances for survival and improved quality of life.
By understanding the causes, risk factors, and modern treatment strategies, individuals can make informed health decisions. Raising awareness and promoting early medical attention for hemoptysis remain essential in the global fight against lung cancer.