Hot flashes are often associated with hormonal changes, particularly in women during menopause. However, many people are surprised to learn that hot flashes can also be linked to certain types of cancer or cancer treatments. While not always a direct symptom of cancer itself, hot flashes may serve as a warning sign that should not be ignored.
Understanding the relationship between hot flashes and cancer can help patients recognize early warning signs, seek medical advice sooner, and manage symptoms more effectively. This article explores the connection between hot flashes symptoms of cancer, their causes, diagnosis, and treatment options, while also offering coping strategies and prevention tips.
Definition and Overview
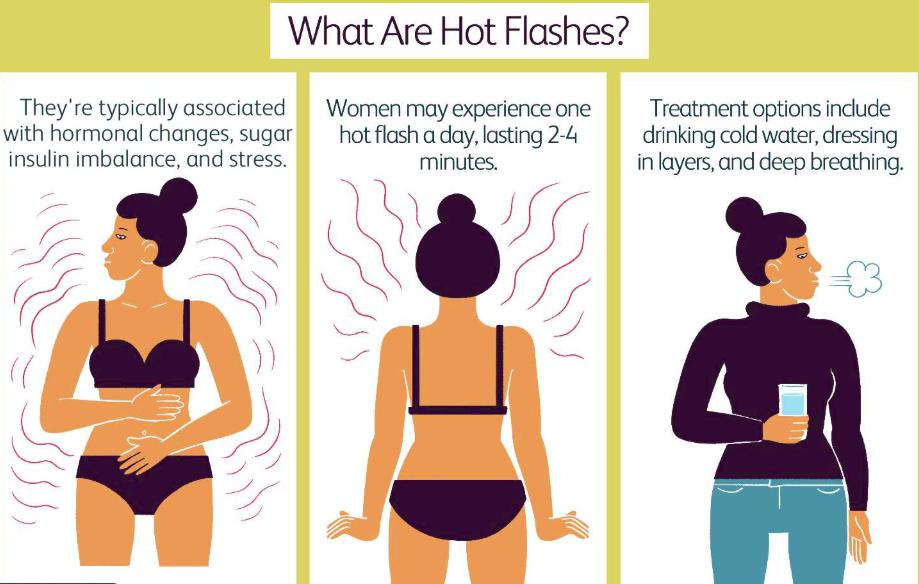
Hot flashes are sudden feelings of warmth, often accompanied by sweating, flushing, and sometimes rapid heartbeat. They are typically triggered by hormonal fluctuations, but in some cases, they can be associated with cancer or its treatment. When considering hot flashes symptoms of cancer, it is important to note that they may occur due to tumors affecting hormone regulation, or as side effects of therapies such as chemotherapy, hormone therapy, or radiation.
Types
There are different types of hot flashes related to cancer and its treatment:
- Hormone-related hot flashes: Caused by tumors that interfere with hormone balance or endocrine function.
- Treatment-induced hot flashes: Often occur in patients undergoing chemotherapy, hormone therapy (like tamoxifen or androgen deprivation therapy), or radiation.
- Secondary hot flashes: Triggered by medications or the stress response associated with cancer.
Causes and Risk Factors
The causes of hot flashes symptoms of cancer vary depending on the condition:
- Hormone-sensitive cancers such as breast, prostate, and ovarian cancers.
- Cancer treatments that reduce estrogen or testosterone levels.
- Medications that disrupt hormonal balance.
- Risk factors include being over 40, undergoing hormone-related cancer treatment, or having a family history of cancer.
Symptoms and Early Warning Signs
Hot flashes associated with cancer may differ slightly from those linked to menopause. Key symptoms include:
- Sudden intense heat in the face, chest, or upper body.
- Excessive sweating, especially at night (night sweats).
- Flushing or reddening of the skin.
- Rapid or irregular heartbeat.
- Dizziness or anxiety during episodes.
When hot flashes occur frequently, at unusual times, or in individuals not typically prone to them, they may point to an underlying medical condition including cancer.
Diagnosis
Diagnosing hot flashes symptoms of cancer involves a thorough evaluation:
- Medical history review to determine frequency, duration, and triggers.
- Blood tests to check hormone levels.
- Imaging tests (CT scans, MRIs, or ultrasounds) to detect tumors affecting endocrine glands.
- Cancer screening tests based on risk factors and age.
Treatment Options
Managing hot flashes linked to cancer depends on the underlying cause:
- Medications: Hormone therapy, antidepressants, or nerve blockers may help.
- Cancer treatment adjustments: Doctors may modify chemotherapy or hormone therapy to reduce hot flashes.
- Alternative therapies: Acupuncture, relaxation techniques, and herbal remedies (under medical guidance).
- Lifestyle changes: Cooling techniques, stress management, and avoiding hot flash triggers.
Prevention and Lifestyle Recommendations
While not all hot flashes can be prevented, certain lifestyle changes may help reduce their severity:
- Maintain a healthy weight and balanced diet.
- Avoid alcohol, caffeine, and spicy foods that may trigger hot flashes.
- Practice relaxation techniques such as yoga, meditation, or deep breathing.
- Keep sleeping environments cool to manage night sweats.
- Stay hydrated and exercise regularly.
Prognosis and Survival Rates
Hot flashes symptoms of cancer are not life-threatening by themselves, but they may indicate an underlying cancer that requires immediate attention. Prognosis depends on the type and stage of cancer, response to treatment, and overall health. Early detection improves survival rates and helps manage symptoms effectively.
Latest Research and Innovations
Recent studies are exploring targeted therapies to minimize treatment-induced hot flashes without compromising cancer care. Advances in hormone regulation, non-hormonal drugs, and integrative medicine are offering new hope for patients experiencing hot flashes symptoms of cancer. Clinical trials continue to investigate safer, more effective methods to reduce these discomforts.
Coping and Support for Patients
Coping with hot flashes can be challenging, especially when combined with cancer treatment side effects. Patients benefit from:
- Support groups and counseling.
- Open communication with healthcare providers.
- Practical strategies like layered clothing, portable fans, and relaxation exercises.
- Professional guidance on dietary and lifestyle adjustments.
Conclusion
Hot flashes symptoms of cancer can serve as important warning signs or treatment side effects. Recognizing them, seeking timely medical evaluation, and adopting effective management strategies can make a significant difference in quality of life. With ongoing research and supportive care, patients can better manage hot flashes and focus on recovery and well-being.
FAQ
Are hot flashes always a sign of cancer?
No, hot flashes are most commonly linked to menopause or hormonal changes, but in some cases, they may be related to cancer or its treatment.
Which cancers are most associated with hot flashes?
Breast cancer, prostate cancer, and ovarian cancer are among the most commonly linked to hot flashes.
Can hot flashes go away after cancer treatment ends?
Yes, in many cases hot flashes improve after treatment, though some patients may experience long-term symptoms.
What should I do if I experience frequent hot flashes with no clear cause?
Consult a healthcare professional to rule out underlying conditions, including cancer.
Are there natural remedies for hot flashes symptoms of cancer?
Yes, lifestyle changes, cooling techniques, and stress management may help, but always discuss alternatives with a doctor before trying them.