Many women facing cervical cancer often wonder, can you get pregnant if you have cervical cancer? This is a deeply personal and important question because cervical cancer not only impacts health but can also affect fertility and family planning. With medical advancements, treatment outcomes and reproductive options have improved, but the situation remains complex.
Cervical cancer is one of the most common gynecological cancers worldwide, and it primarily affects women in their reproductive years. Understanding how this condition interacts with fertility, treatment decisions, and pregnancy is crucial. This article will provide a detailed look into cervical cancer, its impact on fertility, treatment options, and possible paths to parenthood.
Definition and Overview
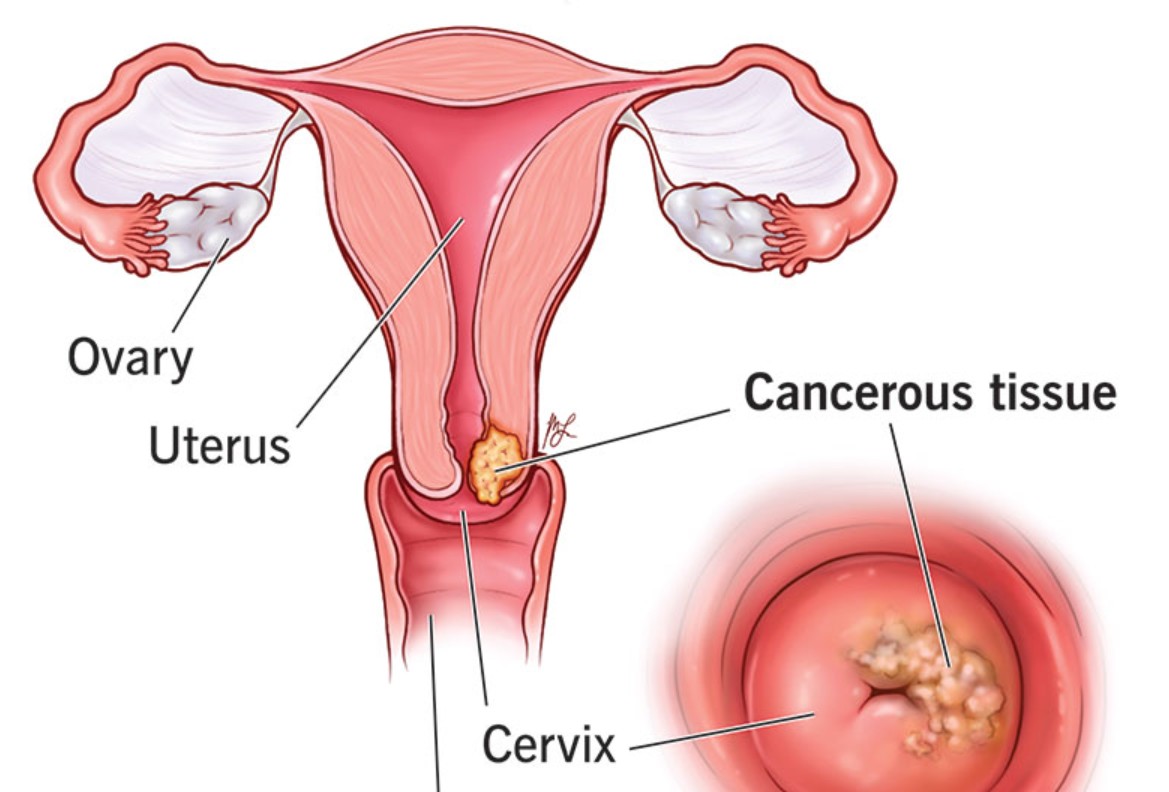
Cervical cancer is a type of cancer that develops in the cells of the cervix, the lower part of the uterus that connects to the vagina. It usually starts with precancerous changes caused by persistent infection with high-risk human papillomavirus (HPV). When untreated, these changes can progress to invasive cancer.
For women of childbearing age, one of the most pressing questions is whether pregnancy is possible before, during, or after treatment. While the disease itself may not directly prevent pregnancy, treatments such as surgery, chemotherapy, or radiation often affect fertility.
Types of Cervical Cancer
Cervical cancer is primarily divided into two major types:
- Squamous cell carcinoma – The most common type, arising in the thin, flat cells lining the cervix.
- Adenocarcinoma – Less common, but increasing in prevalence, originating in the glandular cells of the cervix.
Both types can influence reproductive health depending on the stage, severity, and treatment required.
Causes and Risk Factors
The primary cause of cervical cancer is persistent infection with high-risk HPV types. However, other risk factors can increase the likelihood of developing the disease, including:
- Early onset of sexual activity
- Multiple sexual partners
- Smoking
- Weakened immune system
- Long-term use of oral contraceptives
- Family history of cervical cancer
Understanding these risk factors can help in prevention and early detection.
Symptoms and Early Warning Signs
In its early stages, cervical cancer often presents no symptoms, which makes regular screening essential. As the disease progresses, common symptoms include:
- Abnormal vaginal bleeding (between periods, after intercourse, or postmenopause)
- Unusual vaginal discharge
- Pelvic pain or discomfort during intercourse
- Lower back pain or leg swelling in advanced stages
Recognizing these warning signs early can lead to faster diagnosis and better fertility outcomes.
Diagnosis
Cervical cancer diagnosis typically involves:
- Pap smear to detect abnormal cervical cells
- HPV testing to identify high-risk virus strains
- Colposcopy and biopsy to confirm abnormal changes
- Imaging tests such as MRI, CT, or PET scans for staging
Early diagnosis not only improves survival chances but also provides more fertility-preserving treatment options.
Treatment Options
Treatment depends on the stage of cervical cancer and whether fertility preservation is a priority. Options include:
- Surgery: Cone biopsy or trachelectomy can remove cancer while preserving the uterus, allowing pregnancy to remain possible. Hysterectomy, however, eliminates fertility.
- Radiation therapy: Effective for cancer control but usually damages the ovaries and uterus, leading to infertility.
- Chemotherapy: May be used alongside radiation and can impact ovarian function.
- Targeted therapy and immunotherapy: Emerging treatments may offer new possibilities with less impact on fertility.
If you ask, can you get pregnant if you have cervical cancer, the answer often depends on the stage of cancer, chosen treatment, and whether fertility-preserving procedures are possible.
Prevention and Lifestyle Recommendations
Prevention plays a vital role in reducing the risk of cervical cancer and maintaining reproductive health. Key recommendations include:
- Getting the HPV vaccine at an early age
- Regular Pap smear and HPV tests
- Practicing safe sex
- Quitting smoking
- Maintaining a strong immune system through a healthy lifestyle
These measures not only reduce the risk of cervical cancer but also protect fertility.
Prognosis and Survival Rates
The prognosis of cervical cancer depends on the stage at diagnosis. When detected early, survival rates are high, often exceeding 90% for localized stages. However, advanced stages significantly lower survival rates. Fertility preservation is more feasible in early stages before aggressive treatment is required.
Latest Research and Innovations
Recent research has focused on fertility-sparing treatments such as radical trachelectomy and ovarian transposition. Advances in assisted reproductive technologies (ART), such as IVF and egg freezing, also give women with cervical cancer new possibilities for parenthood. Immunotherapies and targeted drugs are also showing promise in improving survival while minimizing reproductive damage.
Coping and Support for Patients
A cervical cancer diagnosis can be emotionally overwhelming, especially for women concerned about fertility and pregnancy. Support systems, including counseling, fertility specialists, and patient advocacy groups, can help women navigate decisions. Emotional well-being is just as important as physical health in this journey.
Conclusion
So, can you get pregnant if you have cervical cancer? The answer is complex. While cervical cancer itself may not always prevent pregnancy, treatments can significantly affect fertility. With early detection, fertility-preserving treatments, and advances in reproductive medicine, many women can still pursue motherhood.
It is essential to consult both oncologists and fertility specialists before making treatment decisions. Each case is unique, and personalized care offers the best chance to balance cancer treatment with reproductive goals.
FAQ
1. Can you get pregnant while having cervical cancer?
It is possible in very early stages, but pregnancy during active cancer is risky and requires immediate medical consultation.
2. Does cervical cancer treatment always cause infertility?
Not always. Some procedures, like trachelectomy, allow fertility preservation, but radiation and hysterectomy typically cause infertility.
3. Can cervical cancer be detected during pregnancy?
Yes, routine Pap smears during prenatal care can detect cervical abnormalities, and treatment may be adjusted to protect the pregnancy.
4. Is it safe to delay cervical cancer treatment to try for pregnancy?
Delaying treatment is not recommended as it can worsen the prognosis. Fertility preservation methods like egg freezing should be considered before treatment.
5. What fertility options exist after cervical cancer treatment?
Options include IVF, surrogacy, or adoption. Some women may still conceive naturally after fertility-sparing surgery.