Triple negative breast cancer (TNBC) is one of the most aggressive types of breast cancer and is often associated with a higher risk of recurrence compared to other forms. For many patients, the uncertainty surrounding triple negative breast cancer recurrence can be overwhelming, making knowledge and proactive care essential.
Understanding the unique characteristics of TNBC, including its recurrence patterns, is critical for patients, caregivers, and healthcare professionals. By staying informed about risk factors, early warning signs, and treatment options, individuals can make better decisions for long-term health and improved outcomes.
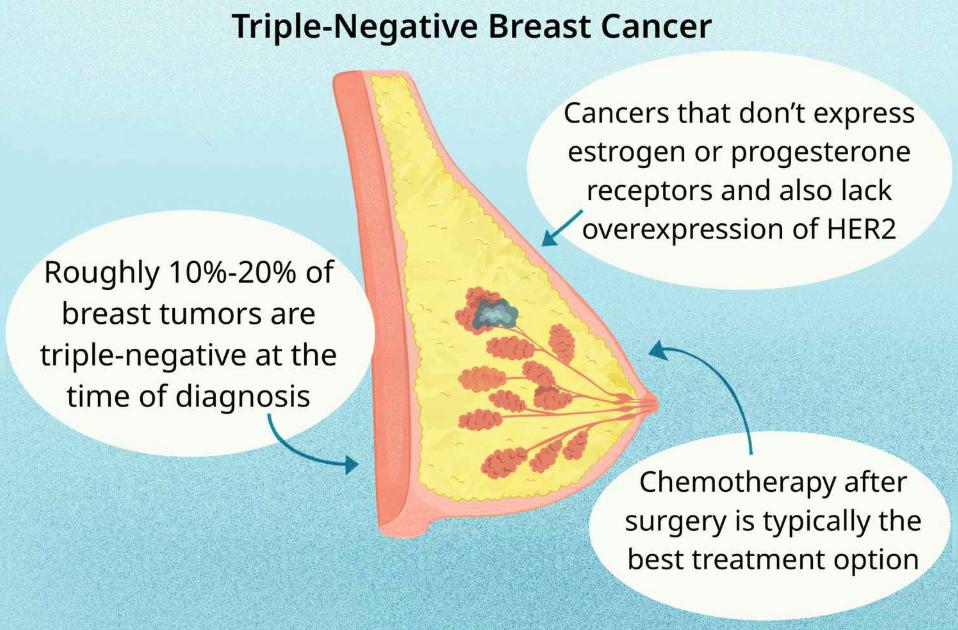
Definition and Overview
Triple negative breast cancer is a subtype of breast cancer that does not express estrogen receptors (ER), progesterone receptors (PR), or HER2 protein. This absence of hormone receptors limits the effectiveness of targeted therapies, making treatment more challenging. Recurrence occurs when cancer returns after treatment, either in the same breast, nearby lymph nodes, or distant organs.
Because TNBC tends to grow and spread faster, recurrence often happens within the first three to five years after initial treatment. After this period, the risk generally decreases, but ongoing monitoring remains important.
Types
Triple negative breast cancer recurrence can be categorized into:
- Local recurrence – when cancer reappears in the same breast or chest wall.
- Regional recurrence – when it spreads to nearby lymph nodes.
- Distant recurrence (metastasis) – when cancer cells travel to organs such as the lungs, liver, or brain.
Each type of recurrence requires a different diagnostic and treatment approach.
Causes and Risk Factors
While the exact cause of triple negative breast cancer recurrence is not fully understood, several risk factors contribute, including:
- Genetics: BRCA1 and BRCA2 gene mutations increase the likelihood of recurrence.
- Age and ethnicity: TNBC is more common in younger women and African-American women.
- Tumor size and stage: Larger tumors or those that have spread to lymph nodes have a higher recurrence risk.
- Incomplete treatment: If initial therapy does not eliminate all cancer cells, recurrence is more likely.
Symptoms and Early Warning Signs
Signs of triple negative breast cancer recurrence vary depending on the type. Common symptoms include:
- A new lump in the breast or chest area
- Swelling in lymph nodes around the armpit or collarbone
- Persistent pain or changes in the breast skin
- Shortness of breath or cough (if spread to lungs)
- Headaches, dizziness, or seizures (if spread to brain)
- Abdominal pain, jaundice, or unexplained weight loss (if spread to liver)
Any unusual or persistent symptoms should be reported to a doctor immediately.
Diagnosis
Doctors use several methods to detect recurrence:
- Imaging tests such as mammograms, ultrasounds, CT scans, or MRIs
- Biopsies to confirm whether a suspicious area is cancerous
- Blood tests to check for tumor markers or liver function abnormalities
- PET scans to detect cancer spread throughout the body
Early diagnosis of recurrence significantly improves treatment options and outcomes.
Treatment Options
Treatment for triple negative breast cancer recurrence depends on the location and severity of the return. Options include:
- Surgery for local recurrence when possible
- Chemotherapy as a primary systemic treatment
- Radiation therapy to target localized tumors
- Immunotherapy and targeted therapies such as checkpoint inhibitors and PARP inhibitors (especially for BRCA mutation carriers)
- Clinical trials offering access to innovative treatments
Prevention and Lifestyle Recommendations
While recurrence cannot always be prevented, patients can take steps to reduce risk and improve overall health:
- Maintain a healthy diet rich in fruits, vegetables, and lean proteins
- Engage in regular physical activity to boost immunity and energy
- Limit alcohol consumption and avoid smoking
- Manage stress through mindfulness, yoga, or counseling
- Adhere to follow-up appointments and screenings for early detection
Prognosis and Survival Rates
The prognosis for triple negative breast cancer recurrence varies. Recurrence within the first few years typically indicates a more aggressive form, but advances in treatment are improving survival rates. Research shows that after five years without recurrence, the chances of long-term survival increase significantly.
Latest Research and Innovations
Scientists are making progress in developing better treatments for TNBC recurrence. Current innovations include:
- PARP inhibitors for patients with BRCA mutations
- Immunotherapy drugs such as checkpoint inhibitors that strengthen the immune response
- Antibody-drug conjugates that deliver chemotherapy directly to cancer cells
- Genomic profiling to personalize treatment plans based on tumor biology
Coping and Support for Patients
Facing triple negative breast cancer recurrence can be emotionally draining. Support strategies include:
- Joining support groups for shared experiences and encouragement
- Seeking professional counseling for anxiety and depression
- Engaging in family and community support networks
- Exploring integrative therapies like meditation, acupuncture, and art therapy to reduce stress
Conclusion
Triple negative breast cancer recurrence remains a serious challenge, but growing awareness and medical advances are providing hope. Understanding risk factors, recognizing early signs, and maintaining a healthy lifestyle can improve outcomes. With continued research and supportive care, patients can face recurrence with resilience and informed decision-making.
FAQ
1. What is the risk of triple negative breast cancer recurrence?
The highest risk is within the first three to five years after treatment, especially for advanced-stage cases.
2. Can lifestyle changes prevent recurrence?
While no lifestyle change guarantees prevention, healthy habits such as regular exercise, balanced nutrition, and avoiding smoking can reduce overall cancer risk.
3. How is recurrence different from metastasis?
Recurrence refers to cancer coming back locally or regionally, while metastasis means the cancer has spread to distant organs.
4. What are the latest treatments for TNBC recurrence?
New therapies include immunotherapy, PARP inhibitors, and antibody-drug conjugates, often available through clinical trials.
5. Should I join a clinical trial if I experience recurrence?
Yes, clinical trials may provide access to cutting-edge treatments not yet widely available, offering new hope for better outcomes.