Breast cancer is a complex disease with many subtypes, each requiring a specific approach to diagnosis and treatment. Among the most common is estrogen receptor positive breast cancer, a form that depends on estrogen, the primary female hormone, to grow and spread. Understanding this type of cancer is crucial because it affects treatment decisions, prognosis, and long-term management.
For patients and families, receiving an estrogen receptor positive breast cancer diagnosis can feel overwhelming. However, with advances in medical research, survival rates are improving, and more treatment options are available than ever before. This article will guide you through everything you need to know, from causes and symptoms to treatment and coping strategies.
Definition and Overview
Estrogen receptor positive breast cancer (ER+ breast cancer) is a subtype of breast cancer where tumor cells have receptors that bind to the hormone estrogen. This means that estrogen fuels the cancer’s growth. Approximately 70% of all breast cancers are ER-positive, making it the most common form of the disease.
Doctors classify breast cancers by their hormone receptor status, which significantly impacts treatment. ER-positive cancers generally respond well to hormone therapy, which blocks or lowers estrogen levels in the body to slow or stop tumor growth.
Types
Estrogen receptor positive breast cancer can be categorized based on several factors:
- ER-positive/PR-positive: Tumors that respond to both estrogen and progesterone hormones.
- ER-positive/PR-negative: Tumors that rely mainly on estrogen.
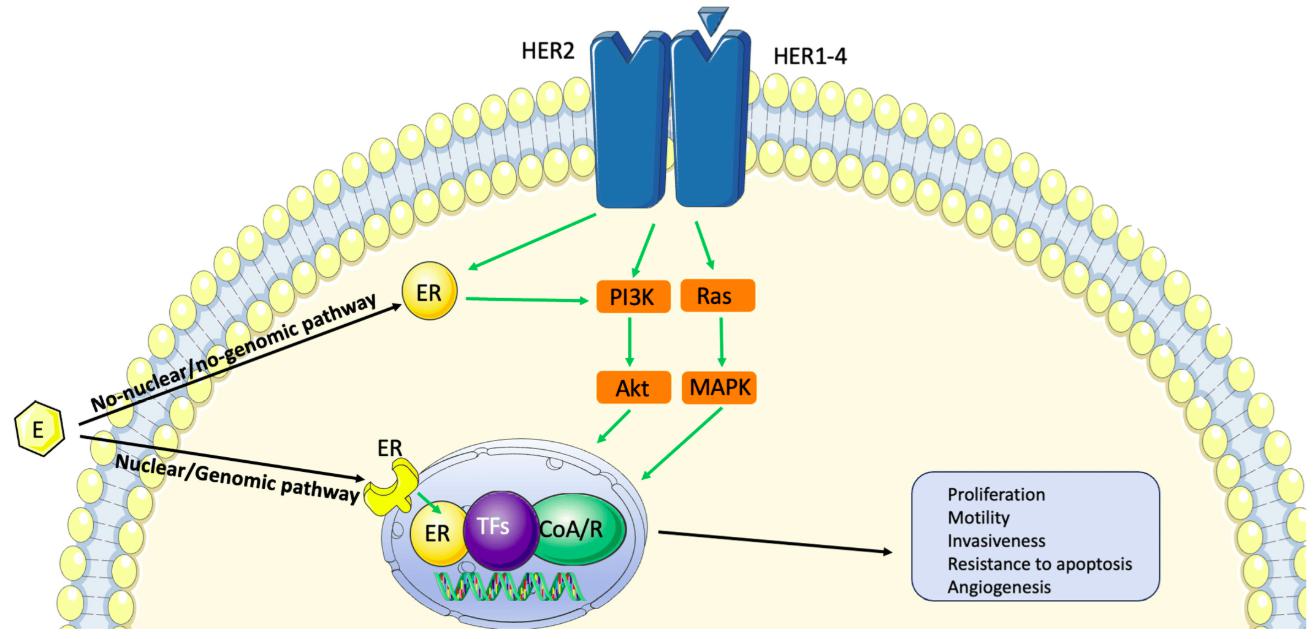
- HER2 status: ER-positive cancers may be HER2-positive or HER2-negative, influencing treatment plans.
Each type responds differently to therapies, making precise classification essential for effective treatment.
Causes and Risk Factors
The exact cause of estrogen receptor positive breast cancer remains unknown, but several factors increase risk:
- Age: Most common in women over 50.
- Hormonal exposure: Long-term exposure to estrogen, such as early menstruation or late menopause.
- Genetics: Family history of breast cancer or BRCA gene mutations.
- Lifestyle factors: Obesity, alcohol use, and lack of physical activity.
- Reproductive history: Never having children or having the first child later in life.
These risk factors do not guarantee cancer development but may raise the likelihood of an ER-positive diagnosis.
Symptoms and Early Warning Signs
Common signs of estrogen receptor positive breast cancer include:
- A lump or thickening in the breast or underarm.
- Changes in breast shape, size, or appearance.
- Unexplained nipple discharge, sometimes with blood.
- Breast pain or tenderness.
- Skin dimpling or redness over the breast.
Early detection through regular screenings and awareness of these symptoms significantly improves treatment success.
Diagnosis
Diagnosis of ER-positive breast cancer involves multiple steps:
- Mammogram and ultrasound to identify abnormalities.
- Biopsy to confirm cancer presence and hormone receptor status.
- Immunohistochemistry (IHC) testing to detect estrogen receptors on tumor cells.
- Staging scans such as MRI, CT, or PET scans to determine cancer spread.
Determining receptor status is critical, as it directly guides the treatment plan.
Treatment Options
Treatment for estrogen receptor positive breast cancer often includes a combination of therapies:
- Hormone therapy (tamoxifen, aromatase inhibitors) to block estrogen activity.
- Surgery (lumpectomy or mastectomy) to remove tumors.
- Radiation therapy to kill remaining cancer cells after surgery.
- Chemotherapy in cases where cancer is aggressive or advanced.
- Targeted therapy for patients with specific tumor markers.
Most patients benefit significantly from hormone therapy, which reduces recurrence risk.
Prevention and Lifestyle Recommendations
While estrogen receptor positive breast cancer cannot always be prevented, lifestyle changes can reduce risk:
- Maintain a healthy weight and balanced diet.
- Engage in regular physical activity.
- Limit alcohol consumption and avoid smoking.
- Discuss hormone replacement therapy risks with a doctor.
- Attend routine mammograms and screenings.
These proactive steps not only lower cancer risk but also improve overall well-being.
Prognosis and Survival Rates
Patients with estrogen receptor positive breast cancer often have a favorable prognosis compared to other breast cancer subtypes. The five-year survival rate is higher when diagnosed early, often exceeding 90%. Long-term outcomes depend on stage, age, treatment response, and overall health. Importantly, ER-positive cancers can recur even years after initial treatment, making long-term monitoring essential.
Latest Research and Innovations
Research in ER-positive breast cancer is rapidly advancing. Current innovations include:
- CDK4/6 inhibitors that improve survival when combined with hormone therapy.
- Genomic testing to tailor treatment to individual patients.
- Immunotherapy trials exploring ways to enhance the immune system’s response.
- Liquid biopsies for detecting recurrence earlier than traditional scans.
These breakthroughs bring hope for more personalized and effective treatment strategies.
Coping and Support for Patients
Living with estrogen receptor positive breast cancer can be emotionally and physically challenging. Patients benefit from:
- Support groups and counseling.
- Education about treatment side effects and self-care.
- Nutrition and exercise programs designed for cancer survivors.
- Family and community support to manage daily stress.
Coping strategies play a vital role in improving quality of life during and after treatment.
Conclusion
Estrogen receptor positive breast cancer is the most common form of breast cancer, but also one of the most treatable thanks to advances in hormone therapy and targeted treatments. Early detection, accurate diagnosis, and comprehensive care are key to achieving the best possible outcomes. By understanding risk factors, recognizing symptoms, and adopting a healthy lifestyle, patients can take proactive steps in prevention and long-term health management.
FAQ
1. What does estrogen receptor positive breast cancer mean?
It means the cancer cells have receptors that allow estrogen to stimulate their growth.
2. Is estrogen receptor positive breast cancer curable?
When detected early, it is highly treatable and often curable, though long-term monitoring is important.
3. What treatments work best for ER-positive breast cancer?
Hormone therapy is the cornerstone of treatment, often combined with surgery, radiation, or chemotherapy.
4. Can men get estrogen receptor positive breast cancer?
Yes, although rare, men can also develop ER-positive breast cancer.
5. Does ER-positive breast cancer come back?
Yes, recurrence is possible even many years after treatment, which is why regular follow-up care is essential.