Bone cancer in dogs is one of the most serious conditions that can affect our canine companions. It often progresses rapidly and causes significant pain, making early detection and accurate diagnosis essential for the best possible outcome. As a responsible pet owner, understanding how bone cancer is diagnosed in dogs can make a crucial difference in recognizing warning signs and seeking timely veterinary care.
Bone cancer, also known as osteosarcoma, primarily affects large and giant dog breeds but can occur in any breed or size. Since its symptoms often mimic less severe conditions like arthritis or injury, it’s important to know how veterinarians determine whether a dog’s bone pain is something more serious. This article provides a comprehensive guide to the diagnosis, treatment, and management of bone cancer in dogs, helping you make informed decisions for your pet’s health.
Definition and Overview
Bone cancer in dogs refers to a malignant tumor that originates in the bones. The most common type is osteosarcoma, accounting for nearly 85% of all canine bone tumors. This cancer tends to be aggressive, spreading rapidly to other parts of the body, especially the lungs and other bones.
Osteosarcoma typically affects the long bones of the legs—such as the humerus, radius, femur, and tibia—but can also occur in the jaw, ribs, or spine. Understanding how bone cancer is diagnosed in dogs is crucial because early intervention can significantly improve a dog’s comfort and survival time.
Types
The main types of bone cancer in dogs include:
- Osteosarcoma (OSA): The most common and aggressive form, affecting both young and older dogs.
- Chondrosarcoma: Originates in cartilage and tends to grow more slowly.
- Fibrosarcoma: Develops from fibrous tissue within the bone.
- Hemangiosarcoma: Arises from blood vessel cells and can involve bones.
- Multilobular Osteochondrosarcoma (MLO): Typically affects the skull and has a mixed bone-cartilage structure.
Causes and Risk Factors
While the exact cause of bone cancer in dogs remains unknown, several risk factors increase susceptibility:
- Breed and size: Large breeds such as Great Danes, Rottweilers, Greyhounds, and Golden Retrievers are more prone.
- Age: Most cases occur in middle-aged to older dogs.
- Previous fractures or bone injuries: Old bone trauma or surgical implants may increase risk.
- Genetics: Certain hereditary factors may predispose dogs to osteosarcoma.
- Gender: Males have a slightly higher incidence than females.
Symptoms and Early Warning Signs
Recognizing the early signs is key to timely diagnosis. Common symptoms of bone cancer in dogs include:
- Persistent limping or lameness
- Swelling near joints or bones
- Pain when touching the affected area
- Reluctance to walk or exercise
- Loss of appetite and weight loss
- Lethargy or fatigue
- In advanced cases, visible lumps or pathological fractures may occur
If your dog shows any of these signs, consult a veterinarian immediately.
Diagnosis
Understanding how bone cancer is diagnosed in dogs involves multiple diagnostic procedures to confirm the disease and rule out other causes. The typical diagnostic steps include:
- Physical Examination: The vet checks for swelling, pain, and mobility issues.
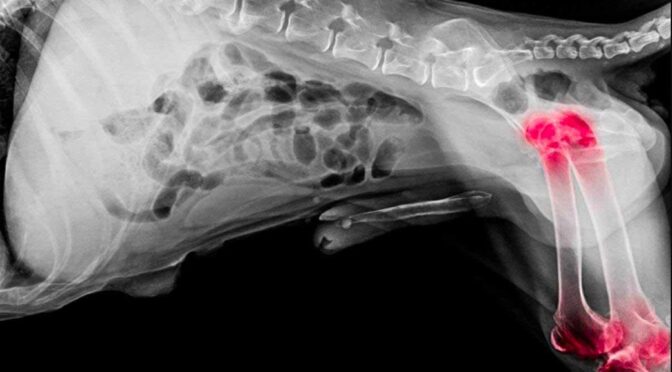
- X-Rays (Radiographs): Bone cancer often shows a distinct pattern of bone destruction and irregular growth.
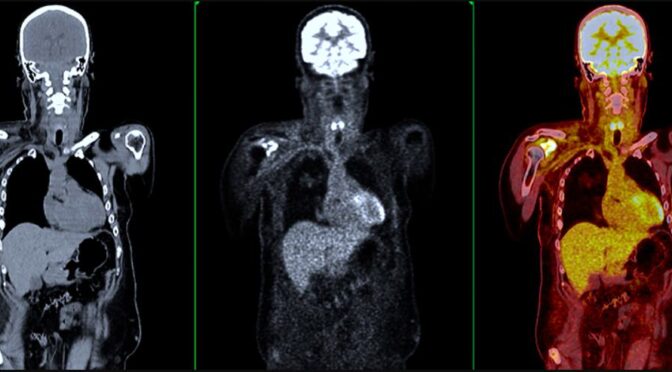
- CT Scan or MRI: Used to assess tumor size, location, and possible spread to other tissues.
- Bone Biopsy: A sample of bone tissue is taken for microscopic examination to confirm cancer type.
- Blood Tests: These help evaluate overall health and detect abnormalities linked to cancer.
- Chest X-Rays: Performed to check for metastasis in the lungs.
Early and accurate diagnosis ensures that treatment can begin before the cancer spreads further.
Treatment Options
Treatment for bone cancer in dogs typically involves a combination of therapies aimed at controlling pain, slowing cancer growth, and improving quality of life. Common treatments include:
- Amputation: Removes the affected limb, eliminating the source of pain and disease in most cases.
- Chemotherapy: Often used after surgery to target remaining cancer cells and prevent spread.
- Radiation Therapy: Helps relieve pain and control tumor growth.
- Limb-Sparing Surgery: Preserves the limb by removing only the tumor and affected bone segment.
- Palliative Care: Focuses on pain management and maintaining comfort for advanced cases.
Prevention and Lifestyle Recommendations
There is no guaranteed way to prevent bone cancer in dogs, but you can reduce risks and promote overall health by:
- Maintaining a balanced diet and healthy weight
- Providing regular exercise without overstraining bones
- Scheduling routine veterinary check-ups
- Monitoring any previous injuries for unusual changes
- Avoiding unnecessary exposure to environmental toxins
Prognosis and Survival Rates
The prognosis for dogs with bone cancer depends on factors such as tumor location, metastasis, and treatment type. With amputation and chemotherapy, the average survival time is 10–12 months, and about 20% of dogs may live two years or longer. Without treatment, most dogs survive only a few months due to rapid disease progression.
Latest Research and Innovations
Recent advances in veterinary oncology have improved outcomes for dogs with bone cancer. Research into targeted therapies, immunotherapy, and novel pain management drugs offers hope for extending survival and improving quality of life. Clinical trials are ongoing to develop safer, more effective treatments with fewer side effects.
Coping and Support for Patients
Caring for a dog with bone cancer is emotionally challenging. Support from veterinary professionals, pet support groups, and online communities can help owners manage both practical and emotional aspects of the journey. Prioritize your dog’s comfort, provide pain relief, and focus on maintaining daily joy and bonding moments.
Conclusion
Understanding how bone cancer is diagnosed in dogs empowers pet owners to take early and decisive action. Through timely diagnosis, modern treatment options, and compassionate care, dogs with bone cancer can still experience meaningful, comfortable lives. Always work closely with your veterinarian to determine the best plan tailored to your dog’s condition and needs.
FAQ
1. What is the first sign of bone cancer in dogs?
The first noticeable sign is usually persistent lameness or limping that doesn’t improve with rest or medication.
2. Can bone cancer in dogs be cured?
While a complete cure is rare, early diagnosis and treatment can extend survival and improve quality of life.
3. How do vets confirm bone cancer?
Veterinarians confirm it through imaging tests such as X-rays or CT scans, followed by a bone biopsy for definitive diagnosis.
4. Does bone cancer spread quickly in dogs?
Yes, osteosarcoma tends to spread rapidly, often reaching the lungs or other bones early in the disease.
5. What breeds are most at risk of bone cancer?
Large and giant breeds like Great Danes, Rottweilers, and Irish Wolfhounds are more commonly affected.
6. How can I support my dog with bone cancer?
Follow your vet’s treatment plan, manage pain effectively, ensure comfort, and provide emotional support through love and companionship.