Stagescancer.net – Dealing with a year/” title=”Baca lebih lanjut tentang cancer”>cancer diagnosis can be overwhelming, and the financial burden of ovarian cancer surgery can only add to the stress. In this comprehensive guide, we will provide insights into the cost associated with ovarian cancer surgery in the United States. Understanding the cost factors, potential expenses involved, and strategies to manage healthcare expenses can help you plan and prepare for the financial impact of surgery.
Whether you are exploring treatment options or have already undergone surgery, it’s important to familiarize yourself with the cost of ovarian cancer surgery. We will discuss the factors that influence the cost, potential out-of-pocket expenses, and resources available to help mitigate the financial impact. Let’s begin by understanding the cost of ovarian cancer surgery and what factors come into play.
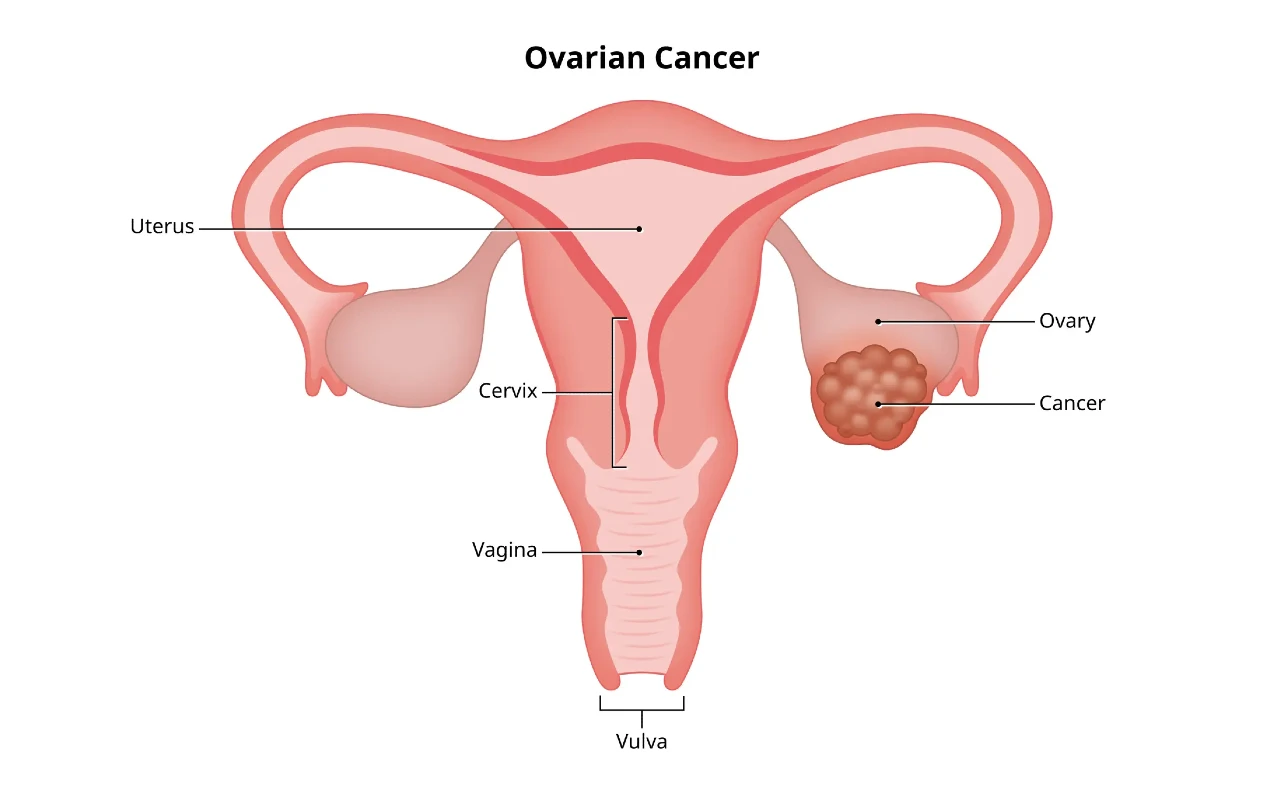
Understanding Ovarian Cancer Surgery
Before delving into the costs, it’s essential to learn about the various types of surgeries for ovarian cancer and their goals. Ovarian cancer surgery depends on factors such as cancer stage, location, and patient health.
Debulking surgery, also known as cytoreductive surgery, is a common procedure for ovarian cancer removal. This surgery involves the removal of the ovary, fallopian tubes, and surrounding tissues. The primary aim is to remove as much cancerous tissue as possible, without affecting healthy organs. The residual cancer left behind after this surgery can be treated later with chemotherapy.
A hysterectomy is a type of surgery that involves removing the uterus and cervix. It is sometimes combined with an oophorectomy, which involves removing one or both ovaries. These surgeries are used for ovarian cancer patients whose cancer is confined to the ovaries and uterus.
If ovarian cancer has spread to other parts of the body, the surgeon may remove the affected organs, such as the spleen, bowel, bladder, or liver. The surgery aims to remove all visible tumors and reduce the cancer burden in the body.
The type of surgery a patient receives cannot be determined until after a diagnosis, during which the surgeon can assess the cancer stage and location. The medical team will, therefore, devise a personalized surgery plan that aligns with cancer treatment goals and patients’ health status.
Impact on Cancer Treatment
Ovarian cancer surgery plays a significant role in determining the course of cancer treatment. Surgery can reduce cancer burden, improve chemotherapy efficacy, and sometimes offer a complete cancer cure, especially if cancer is confined to the ovaries.
However, surgery may also come with side effects and risks, such as bleeding, infection, injury to surrounding organs, or blood clots. The surgeon will discuss these risks and complications with the patient for informed decision-making.
Factors Affecting Ovarian Cancer Surgery Cost
Ovarian cancer surgery costs vary based on several factors that patients should consider when estimating the potential out-of-pocket expenses.
Stage of Cancer
The stage and severity of ovarian cancer can impact the complexity of the surgery and potential additional treatments required. For instance, patients with advanced-stage ovarian cancer may require extensive and complicated debulking surgery, leading to higher costs.
Complexity of Surgery
The complexity of the surgery required to treat ovarian cancer can also contribute to the cost. For instance, surgeons may need to perform a hysterectomy, oophorectomy, or lymph node removal, all of which can be expensive procedures.
Hospital or Facility
The hospital or facility chosen for ovarian cancer surgery also affects the cost. Private hospitals or specialized medical centers may have higher fees and service charges, whereas public hospitals may have reduced fees or discounted rates for uninsured patients.
Additional Treatments Required
In addition to surgical costs, ovarian cancer patients may require additional treatments, such as chemotherapy or radiation therapy. These treatments can also add up to the overall cost of ovarian cancer care.
Average Cost of Ovarian Cancer Surgery
Ovarian cancer surgery costs can vary based on several factors and can range from a few thousand to tens of thousands of dollars. The cost may include expenses for surgery, hospitalization, anesthesia, healthcare provider fees, medications, and other additional treatments required depending on the stage of cancer. The average cost of ovarian cancer surgery in the United States is around $19,000, but it can be as high as $60,000 or more for complex cases requiring multiple surgeries or longer hospital stays.
Cost Ranges for Different Types of Surgeries
The cost of ovarian cancer surgery depends on several factors, including the type of surgery performed. Below is an estimate of the average cost range for each type of surgery:
| Type of Surgery | Average Cost Range |
|---|---|
| Debulking surgery | $15,000 – $50,000 |
| Hysterectomy | $10,000 – $20,000 |
| Oophorectomy | $5,000 – $10,000 |
The cost range may vary depending on the complexity of the surgery, the healthcare provider’s fees, and the specific geographic location. Additional expenses can also occur based on required tests, follow-up care, and medications.
Potential Financial Implications
The cost of ovarian cancer surgery can have significant financial implications for patients and their families. High out-of-pocket expenses, including deductibles, copays, and coinsurance, can place a significant burden on finances. In some cases, individuals may be forced to delay or forego treatment due to the high costs. It’s essential to explore options, including insurance coverage and financial assistance programs, to help manage expenses and provide necessary care.
Having health insurance is crucial in managing the cost of ovarian cancer surgery. Most health insurance plans cover a portion of the cost, and some plans may cover the entire expense. If insurance coverage is not available, individuals can explore financial assistance programs offered by healthcare facilities, non-profit organizations, and government agencies.
In summary, while every case of ovarian cancer is unique, the average cost of surgery in the United States is around $19,000. Understanding the cost ranges for different types of surgeries and the potential financial implications is only the first step in navigating the cost of ovarian cancer surgery. Further sections in this article will provide insights into how to prepare for and manage the financial aspects of this critical treatment.
Preparing for Ovarian Cancer Surgery Costs
Planning for the expenses associated with ovarian cancer surgery can provide clarity and reduce stress. Here are some tips to help you prepare for the financial aspects of your surgery:
Understand your insurance coverage
Review your insurance plan and understand what services are covered and what your out-of-pocket expenses might be. Contact your insurance company to ask for a detailed explanation of all services related to your surgery. Keep notes, names, and dates for every conversation with your insurance provider.
Explore financial assistance options
Many financial assistance programs are available for cancer patients to support them facing cancer treatments. Charitable organizations, local governmental services, and medical centers can provide financial aid, grants, income-based discounts, and scholarships for cancer patients. Apply early, since some programs have specific deadlines or deadlines soon after diagnosis.
Create a budget
Creating a budget is vital to managing cancer-related costs. Document all of your expenses related to your surgery, such as traveling, lodging, and food, and track all invoices and receipts. Consider working with a financial planner or consulting with other women who have had similar surgeries for advice on managing these costs.
“We were able to apply for financial aid and receive some help for my fertility preservation procedure, which was very helpful. Don’t be afraid to ask – assistance is out there, and you deserve it.”
Insurance Coverage for Ovarian Cancer Surgery
Managing the cost of ovarian cancer surgery can be overwhelming, but insurance coverage can provide financial relief. Understanding your coverage options and verifying potential expenses can help you prepare financially and make informed decisions.
Types of Insurance Coverage
Different types of insurance coverage may apply to ovarian cancer surgery, such as:
- Private Health Insurance: Depending on your plan, private health insurance may cover some or all of the expenses associated with ovarian cancer surgery.
- Medicare: Medicare, a federal health insurance program for people over 65 or with certain disabilities, may cover a portion of the cost of ovarian cancer surgery.
- Medicaid: Medicaid, a healthcare program for low-income individuals and families, may offer coverage for ovarian cancer surgery.
Each insurance plan may have different coverage limitations, so it is best to consult with your insurance provider to determine the specific benefits and potential out-of-pocket expenses.
Verifying Your Insurance Coverage
Before undergoing ovarian cancer surgery, it is crucial to verify your insurance coverage to ensure that you understand the scope of your benefits. Here are some steps to follow:
- Contact your insurance provider to obtain a comprehensive list of covered expenses and potential out-of-pocket costs.
- Inquire if there are any out-of-network or non-covered expenses and if you will need to pay for them.
- Confirm if prior authorization is needed for ovarian cancer surgery or any associated treatments or follow-up care.
- Ensure that your healthcare provider is part of your insurance plan’s network to avoid additional expenses.
Potential Out-of-Pocket Expenses
Even with insurance coverage, there may be some potential out-of-pocket expenses associated with ovarian cancer surgery, such as co-pays, deductibles, and coinsurance. It is important to be aware of these additional costs and budget for them accordingly.
Potential Out-of-Pocket Expenses
Undergoing ovarian cancer surgery can result in several potential out-of-pocket expenses in addition to the surgical cost. Being aware of these expenses can help you prepare and effectively manage your healthcare budget.
Pre-Surgery Costs
Before undergoing surgery, your doctor may require several pre-surgery tests to assess your health and determine the best course of treatment. These tests may include blood work, imaging scans, and other diagnostic tests. Costs associated with these tests can vary and may not be fully covered by insurance, resulting in potential out-of-pocket expenses.
Medications
Following surgery, you may require prescription medications to manage pain or prevent infections. These medications may not be fully covered by insurance, resulting in potential out-of-pocket expenses. Additionally, if you have a high-deductible insurance plan, you may be responsible for paying the full cost of these medications until you reach your deductible.
Follow-Up Care
After surgery, it’s essential to attend follow-up appointments with your doctor to monitor your recovery and assess any potential complications. These appointments may involve additional testing, such as blood work or imaging scans, which can result in additional out-of-pocket expenses. Additionally, if you require ongoing therapies such as chemotherapy, radiation, or hormone therapy, these treatments can result in further potential out-of-pocket expenses.
Rehabilitation
Depending on the type and extent of surgery, you may require rehabilitation, such as physical therapy, occupational therapy, or speech therapy, to regain strength, mobility, or other bodily functions. These services may not be fully covered by insurance, possibly resulting in further potential out-of-pocket expenses.
By understanding the potential out-of-pocket expenses associated with ovarian cancer surgery, you can take steps to prepare financially and make informed decisions about your healthcare. Conducting thorough research, assessing insurance coverage, and exploring options for financial assistance can help you manage these costs effectively.
Financial Assistance Programs
Dealing with the financial burden of ovarian cancer surgery is challenging, but there are resources available to provide financial assistance. If you’re struggling with healthcare expenses, here are some financial assistance programs you can explore:
Government Assistance Programs
The federal and state government offers various aid programs to help with medical expenses. Medicaid and Medicare may provide coverage for eligible individuals, while the Department of Health and Human Services offers grants and benefits programs for cancer patients. Check with your local health department to see what programs are available in your area.
Non-profit Organizations
Several non-profit organizations focus on providing financial assistance to cancer patients, such as Cancer Care and the American Cancer Society. These organizations may offer grants, scholarships, or financial assistance programs for healthcare expenses.
Patient Advocacy Groups
Many patient advocacy groups offer financial assistance and support for ovarian cancer patients. These organizations may provide guidance on managing healthcare costs, offer support groups, or connect you with financial assistance programs.
Remember, dealing with the financial impact of ovarian cancer surgery can be overwhelming, but there are resources available to help. Take the time to research financial assistance programs and support options to ease the burden of healthcare expenses.
Negotiating Ovarian Cancer Surgery Costs
Managing the financial burden of ovarian cancer surgery can be overwhelming. Negotiating with healthcare providers and reviewing medical bills can help lower the cost and ease the strain on your finances.
How to negotiate with healthcare providers
When negotiating with healthcare providers, explain your financial situation and ask for a payment plan or a discounted rate. You can also research the fair price for your procedure and ask the provider to match it. Be polite and firm in your approach, and don’t hesitate to seek help from a patient advocate or a financial counselor.
Importance of reviewing medical bills
It’s important to review your medical bills carefully to ensure that you are not overcharged. You can check for errors or unnecessary charges and ask for an explanation if something seems unclear. You can also negotiate with your provider for a lower rate if a charge seems unreasonable.
Potential options for cost reduction
There are various options for cost reduction, such as seeking financial assistance from non-profit organizations or exploring crowdfunding platforms. You can also consider medical tourism, which involves seeking treatment in a foreign country where the cost of care is lower. However, it’s important to research possibilities carefully and weigh the risks and benefits before making a decision.
Medical Tourism for Ovarian Cancer Surgery
For some women, seeking ovarian cancer surgery abroad may be a more cost-effective option. Medical tourism, the practice of traveling to another country for medical treatment, is a growing trend that offers potential savings.
Considerations for Medical Tourism
Before exploring international options, it’s important to do thorough research to assess the risks and benefits. Factors to consider:
- Language barriers
- Cultural differences
- Travel and lodging expenses
- Availability of follow-up care
- Quality and safety standards of the medical facility
It’s important to ensure that the chosen facility meets stringent international healthcare standards and has experienced, qualified surgeons.
Cost Comparison for Ovarian Cancer Surgery
Different countries may offer varying prices for ovarian cancer surgery. It’s essential to compare the potential savings with the total costs, including travel, lodging, and follow-up care.
| Country | Average Cost of Ovarian Cancer Surgery |
|---|---|
| India | $3,000 – $7,000 |
| Mexico | $6,000 – $9,000 |
| Thailand | $5,000 – $8,000 |
| Costa Rica | $7,000 – $12,000 |
Preparing for Medical Tourism
Before deciding to pursue medical tourism for ovarian cancer surgery, there are several preparations to consider:
- Consult with a healthcare provider in your home country to discuss the potential risks and benefits of medical tourism.
- Research and compare healthcare facilities and surgeons in different countries.
- Understand the legal and regulatory requirements for medical tourism in your home country and the destination country.
- Ensure that the chosen healthcare facility can provide all necessary medical records and documentation for follow-up care.
Medical tourism for ovarian cancer surgery can offer potential cost savings, but it’s important to research and plan carefully before making a decision. With the right resources and precautions in place, women can find quality care at a more affordable price.
Managing Post-Surgery Expenses
Ovarian cancer surgery can lead to significant post-surgery expenses, including follow-up appointments, therapies, and long-term care. To manage these costs, it’s essential to plan and have a comprehensive understanding of your healthcare needs.
First, discuss your follow-up care with your healthcare provider. They can guide you on the frequency and types of appointments needed to monitor your recovery and ensure optimal health. Additionally, book appointments well in advance to avoid last-minute expenses and take advantage of any discounts available.
Depending on your cancer treatment plan, ongoing therapies like chemotherapy or radiation may be necessary. These treatments can also result in a considerable financial burden. If your insurance doesn’t cover all the costs, inquire about financial assistance programs that can help you manage the expenses.
| Types of Ongoing Therapies | Cost |
|---|---|
| Chemotherapy | $14,000-$30,000 per year |
| Radiation | $10,000-$50,000 per year |
In some cases, long-term care may also be required, such as rehabilitation services or home health aids. These expenses can quickly add up, impacting your financial stability. Look into financial assistance programs and government care options that can help ease the burden and provide access to necessary care.
Lastly, creating a budget and tracking expenses can help you manage post-surgery costs effectively. Keep a detailed record of medical bills, receipts, and insurance claims to ensure accuracy and avoid overpaying.
Key Takeaways
- Plan for follow-up care and therapies to manage post-surgery expenses
- Explore financial assistance programs and government care options
- Create a budget and track expenses to avoid overpaying
Planning for the Unforeseen
It’s important to prepare for unexpected circumstances that may arise during or after your ovarian cancer surgery. Having a financial contingency plan in place can ease the burden of unforeseen expenses. Consider creating an emergency fund, which can provide additional financial support if complications arise.
Another option is to explore supplemental insurance, which can cover some of the costs associated with unforeseen events. This insurance can provide added financial security and peace of mind.
You can also consider crowdfunding as an option for additional financial assistance. Several crowdfunding platforms now cater specifically to medical bills and can connect you with people willing to contribute to your expenses.
By having a financial contingency plan in place, you can focus on your health and recovery with confidence, knowing that unforeseen expenses will not add more stress to your journey.
Researching Healthcare Providers and Facilities
Choosing the right healthcare provider and facility can significantly impact the success of your ovarian cancer surgery. Before deciding, it’s essential to conduct thorough research to ensure that the healthcare professionals and facility you choose can provide the expertise, quality, and care you need.
Evaluating Surgeon Expertise
One crucial factor to consider is the surgeon’s expertise in performing ovarian cancer surgeries. You can ask your primary care physician for recommendations or search online for board-certified gynecologic oncologists or general surgeons who specialize in ovarian cancer surgery.
Once you’ve found potential surgeons, evaluate their expertise and qualifications by considering factors such as:
- Years of experience in performing ovarian cancer surgeries
- Training and certifications
- Success rates of surgeries performed
- Number of surgeries performed annually
- Specializations, if any
Assessing Healthcare Facility Quality
It’s crucial to choose a healthcare facility that provides high-quality care, maintains a good reputation, and offers the necessary resources for ovarian cancer surgery. Some factors you can consider when assessing facility quality include:
- Certification and accreditation by reputable organizations
- Number of surgeries performed annually
- Availability of necessary equipment and technology
- Qualifications and experience of the support staff
- Patient outcomes and satisfaction rates
Understanding Cost Differences
The cost of ovarian cancer surgery can vary significantly, depending on the healthcare provider and facility you choose. However, it’s essential to remember that cost is not always synonymous with quality. Research and compare different providers and facilities before making a decision.
| Facility Type | Average Cost Range |
|---|---|
| Hospital | $10,000 to $100,000 or more |
| Clinic | $5,000 to $30,000 or more |
| Outpatient Facility | $2,000 to $10,000 or more |
Remember to consider all potential costs, including tests, medications, post-surgery care, and rehabilitation. Some facilities may offer packages that include the entire process.
Researching and evaluating healthcare providers and facilities may take time and effort, but it is crucial to ensure the best outcome from your ovarian cancer surgery.
Emotional and Psychological Support
Dealing with the financial burden of ovarian cancer surgery can take a significant toll on your emotional and psychological well-being. It’s essential to seek emotional support and coping strategies to help you navigate this challenging time.
Connecting with a support group of individuals who have gone through similar experiences can provide a valuable source of emotional support. You may also benefit from counseling or therapy with a mental health professional who specializes in cancer-related issues.
It’s important to share your concerns and feelings with your healthcare team. They can provide guidance and resources to help you manage the emotional impact of surgery costs.
Remember to prioritize self-care and focus on activities that promote your overall well-being, such as exercise, meditation, and hobbies you enjoy. Taking care of your mental and emotional health is just as essential as taking care of your physical health.
Conclusion
Cancer surgery can be a stressful and overwhelming experience, especially when considering the associated costs. Understanding the factors that contribute to the cost of ovarian cancer surgery is an essential step in managing healthcare expenses. By preparing for the costs, exploring insurance options, and utilizing financial assistance programs, you can alleviate the financial burden and focus on your recovery. Remember to research healthcare providers and facilities, seek emotional support, and plan for unforeseen circumstances. With the right strategies in place, you can approach cancer surgery with confidence and peace of mind, knowing that you are prepared to manage the financial implications effectively.
FAQ
How much does ovarian cancer surgery cost?
The cost of ovarian cancer surgery can vary depending on several factors, including the type of surgery, the stage of cancer, and the chosen hospital or facility. On average, the cost ranges from $20,000 to $100,000.
What types of surgeries are involved in ovarian cancer treatment?
Ovarian cancer surgery may include debulking surgery, which involves removing tumors and reducing their size, hysterectomy, which involves removing the uterus, and oophorectomy, which involves removing the ovaries. The specific type of surgery depends on the stage and type of cancer.
What factors can affect the cost of ovarian cancer surgery?
Several factors can influence the cost of ovarian cancer surgery, including the complexity of the surgery, the stage of cancer, the chosen hospital or facility, and the need for additional treatments such as chemotherapy or radiation therapy.
What is the average cost of ovarian cancer surgery?
The average cost of ovarian cancer surgery in the United States ranges from $20,000 to $100,000. However, it is important to note that actual costs can vary depending on individual circumstances and factors.
How can I prepare for the expenses associated with ovarian cancer surgery?
To prepare for the expenses of ovarian cancer surgery, it is advisable to understand your insurance coverage, explore financial assistance programs, and create a budget. It is also important to communicate with your healthcare team about any financial concerns you may have.
Does insurance cover the cost of ovarian cancer surgery?
Insurance coverage for ovarian cancer surgery varies depending on the type of insurance you have. Private health insurance, Medicare, and Medicaid may provide coverage, but it is important to verify your coverage and understand potential out-of-pocket expenses.
What are the potential out-of-pocket expenses associated with ovarian cancer surgery?
In addition to the surgical cost, there may be other out-of-pocket expenses such as pre-surgery tests, medications, follow-up care, and rehabilitation. It is essential to be aware of these potential costs and plan accordingly.
Are there any financial assistance programs available for ovarian cancer surgery?
Yes, there are financial assistance programs available to help individuals with the cost of ovarian cancer surgery. These programs include government assistance programs, non-profit organizations, and patient advocacy groups that offer financial aid, grants, or scholarships.
Can I negotiate the cost of ovarian cancer surgery?
It may be possible to negotiate the cost of ovarian cancer surgery with healthcare providers. It is advisable to be proactive, review medical bills, and explore potential options for cost reduction.
What is medical tourism for ovarian cancer surgery?
Medical tourism refers to traveling to another country to seek more affordable medical treatment, including ovarian cancer surgery. It is important to carefully consider factors such as the reputation and quality of healthcare facilities before considering this option.
How can I manage post-surgery expenses?
Managing post-surgery expenses involves planning for follow-up appointments, ongoing therapies, and potential long-term care. It is important to utilize available resources, such as support groups, to help navigate these financial burdens.
Should I plan for unforeseen complications or emergencies related to ovarian cancer surgery?
Yes, it is important to have a financial contingency plan in case of unforeseen complications or emergencies. This may involve building an emergency fund, considering supplemental insurance, or exploring crowdfunding options to address any unexpected financial challenges.
How can I research healthcare providers and facilities for ovarian cancer surgery?
Researching healthcare providers and facilities for ovarian cancer surgery involves evaluating the expertise of surgeons, assessing the reputation and quality of healthcare facilities, and considering potential cost differences between providers. Online resources, reviews, and recommendations can be helpful in this process.
Is emotional and psychological support available for dealing with the financial burden of ovarian cancer surgery?
Yes, seeking emotional and psychological support is important when facing the financial burden of ovarian cancer surgery. Support groups, mental health professionals, and counselors can provide guidance and assistance in navigating these challenges.