Stagescancer.net – If you or a loved one has been diagnosed with pleural effusion and cancer, one of the first questions that may come to mind is, “What is the life expectancy?” While there is no easy answer, the prognosis for this condition depends on various factors. In this section, we will explore the topic of pleural effusion cancer life expectancy in detail, discussing the impact of cancer stage, type of cancer, and treatment options on overall survival. We hope that this information will help you make informed treatment decisions and provide some peace of mind as you navigate this challenging time.
Understanding Pleural Effusion and Cancer
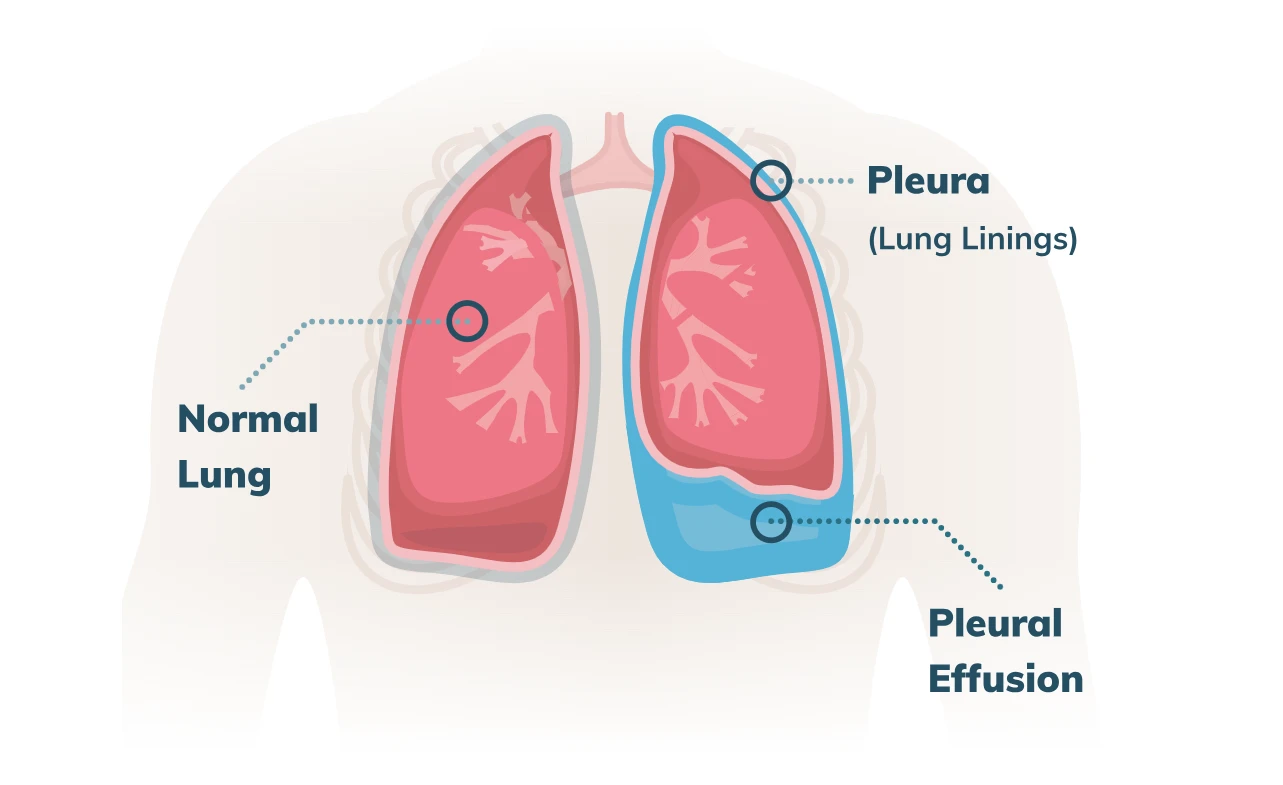
When cancer affects the lining surrounding the lungs, called the pleura, it can cause a buildup of fluid known as pleural effusion. This condition can lead to discomfort, breathing difficulties, and other health complications for cancer patients.
Early diagnosis of pleural effusion is essential to ensure prompt treatment and improve overall prognosis. Common diagnostic tests include imaging scans, such as X-rays or CT scans, and thoracentesis, a procedure in which a needle is inserted into the chest to remove fluid for analysis.
The presence of pleural effusion can also impact treatment decisions for cancer patients, as it may affect the choice of chemotherapy, radiation therapy, or other interventions. By understanding the relationship between cancer and pleural effusion, patients and healthcare providers can make informed decisions about the most appropriate course of action.
Factors Affecting Pleural Effusion Cancer Life Expectancy
The life expectancy of individuals with pleural effusion and cancer depends on several factors that have been identified by medical professionals. These factors can be broadly classified into two categories, primary and secondary.
Primary Factors
The primary factors which influence the life expectancy of individuals diagnosed with pleural effusion cancer are:
| Factor | Description |
|---|---|
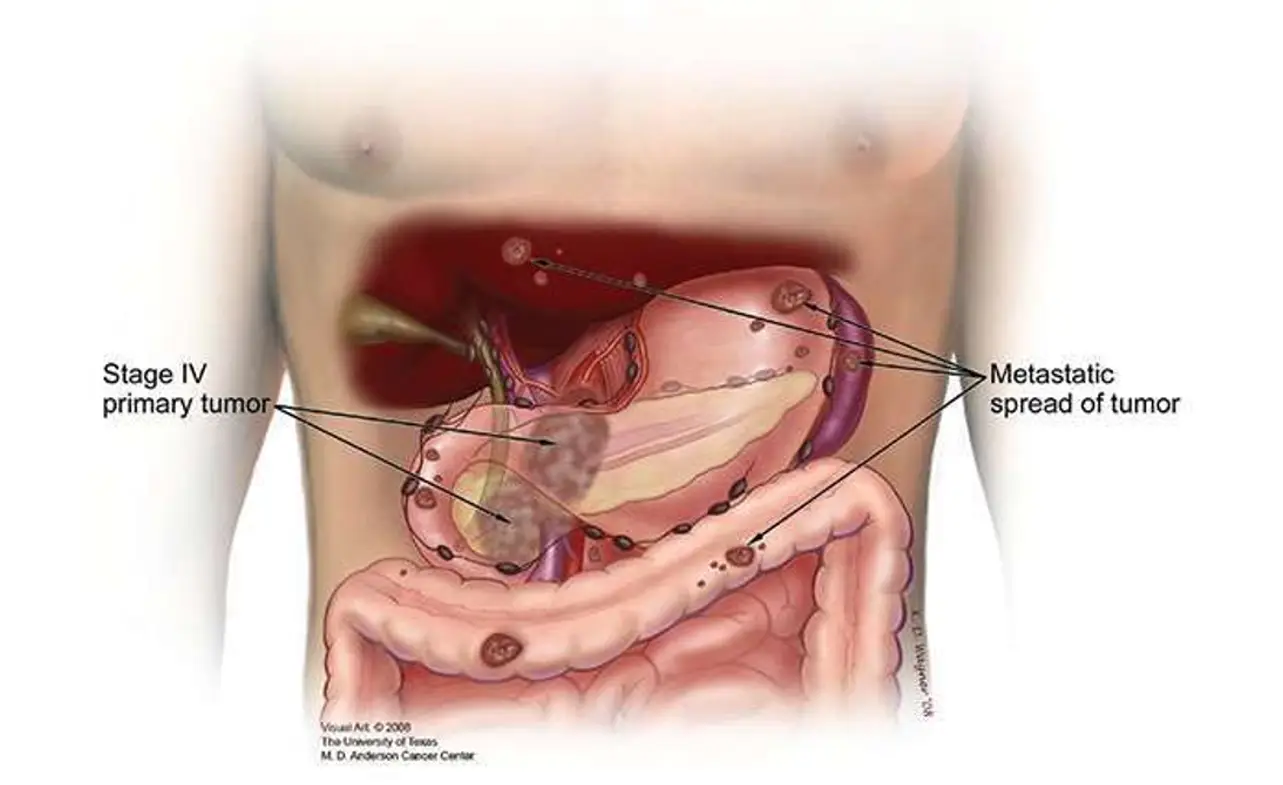
| Cancer Stage | The stage of cancer at the time of diagnosis plays a significant role in determining the life expectancy of patients. |
| Cancer Type | The type of cancer that has caused the pleural effusion is a crucial factor in predicting life expectancy. Some types of cancer, especially those that are more aggressive, may have a lower life expectancy than others. |
| Pleural Fluid Build-up | The rate and extent of pleural fluid build-up is another important factor to consider. Some patients may experience rapid fluid accumulation, which can worsen their prognosis, while others may have a slower rate of fluid build-up. |
| Pleural Effusion Cause | The underlying cause of pleural effusion, such as cancer or infection, can also impact life expectancy. |
Secondary Factors
Secondary factors can also influence the life expectancy of individuals with pleural effusion and cancer. These include:
- Age and overall health of the patient
- Response to treatment
- Effectiveness of palliative care
- Emotional support and mental health
It is important to note that each patient’s situation is unique and multifactorial. Therefore, the impact of these factors may vary from person to person.
Prognosis and Survival Rates for Pleural Effusion Cancer Patients
The prognosis for cancer patients with pleural effusion can vary greatly depending on various factors. According to recent statistics, the estimated 5-year survival rate for all types of lung cancer is around 21%, while the survival rate for pleural mesothelioma specifically is much lower at around 10%.
Other factors that can impact prognosis include the stage of cancer at diagnosis, as well as the type and location of the cancer. For example, if a patient is diagnosed with early-stage lung cancer, their prognosis may be more favorable than if they are diagnosed with advanced-stage mesothelioma.
It is important to note that while statistics can provide a general idea of prognosis, they are not always indicative of an individual’s unique circumstances. Each case is different, and factors such as age, overall health, and response to treatment can all have an impact on life expectancy.
Predicting Prognosis
Healthcare professionals use various tools to predict cancer prognosis, including imaging tests and laboratory analyses. Some of the most common factors used to determine prognosis include:
- Tumor size
- Lymph node involvement
- Stage of cancer
- Type and location of cancer
- Overall health and age of the patient
Factors Affecting Survival Rates
In addition to prognosis, various factors can impact the survival rates of cancer patients with pleural effusion. Some of these factors include:
- Response to treatment
- Presence of other health conditions
- Length of time between diagnosis and treatment
- Age and overall health of the patient
It is important to work closely with healthcare professionals to monitor the impact of these and other factors on prognosis and survival rates.
Treatment Options for Pleural Effusion Cancer
When it comes to treating pleural effusion in cancer patients, there are several options available. The course of treatment will depend on various factors, including the type of cancer, stage of cancer, and overall health of the patient. Here are some of the most common treatment options:
Surgical Procedures
In some cases, surgical intervention may be necessary to treat pleural effusion. This may involve removing fluid from the pleural space or performing a pleurodesis, which is a procedure that seals the pleural space to prevent fluid build-up. Your doctor will determine if surgery is the best course of action for your specific case.
Chemotherapy
Chemotherapy is a common treatment option for cancer patients, and it can also be effective in reducing the amount of fluid in the pleural space. Chemotherapy works by targeting and killing cancer cells, which can alleviate symptoms of pleural effusion. However, chemotherapy can also have significant side effects, and it may not be suitable for all patients.
Radiation Therapy
Like chemotherapy, radiation therapy can also be used to treat cancer and reduce fluid build-up in the pleural space. Radiation therapy uses high-energy radiation to target and kill cancer cells. This treatment option may be used in combination with other therapies or as a standalone treatment.
Other Interventions
In addition to surgery, chemotherapy, and radiation therapy, there are other potential interventions for treating pleural effusion in cancer patients. For example, thoracentesis is a procedure that involves removing fluid from the pleural space using a needle and syringe. Similarly, a chest tube may be inserted to drain fluid from the pleural space over an extended period.
It is essential to work closely with your doctor to determine the best course of treatment for your specific case. In some cases, a combination of therapies may be necessary to manage pleural effusion effectively. Your medical team will carefully monitor your progress and adjust your treatment plan as needed to ensure the best possible outcome.
Impact of Treatment on Pleural Effusion Cancer Life Expectancy
Treatment options for pleural effusion and cancer can have a significant impact on patient outcomes and life expectancy. The most effective treatment approach depends on various factors, including the stage and type of cancer, overall patient health, and personal preferences.
Surgical procedures, such as thoracentesis and pleurodesis, can provide relief from symptoms by draining excess fluid from the pleural space. Chemotherapy and radiation therapy are also common treatment options that can help shrink tumors and slow the progression of cancer.
However, while these treatments can prolong life expectancy and improve the quality of life for some patients, they may not be appropriate or effective in all cases. Moreover, these treatments can have significant side effects that impact overall health and well-being.
Individuals with pleural effusion and cancer must discuss treatment options with their healthcare team. Working together, patients and their doctors can develop a personalized treatment plan that takes into account the patient’s specific needs and goals.
Managing Symptoms and Improving Quality of Life for Pleural Effusion Cancer Patients
Individuals diagnosed with pleural effusion and cancer may experience a range of symptoms that impact their quality of life. Fortunately, there are several strategies and interventions available to manage symptoms and improve overall well-being.
Palliative Care
One approach to managing symptoms and improving quality of life is through palliative care. This specialized care is designed to address the physical, emotional, and spiritual needs of individuals with serious illnesses, such as cancer. Palliative care can help manage pain, alleviate nausea, and provide emotional support to patients and their families.
Pain Management
For those experiencing pain related to pleural effusion, pain management strategies can be effective in improving quality of life. This can include the use of medication to manage pain or the use of non-pharmacological interventions, such as heat therapy or massage.
Supportive Therapies
Supportive therapies, such as physical therapy or occupational therapy, can help manage symptoms and maintain functionality in daily life. These therapies can also provide emotional support and education on how to improve overall quality of life.
Emotional Support
Receiving emotional support is crucial for individuals with pleural effusion and cancer, as it can help improve overall quality of life. Support can come from healthcare professionals and supportive care services, as well as from family and friends. Support groups can also be beneficial as they offer a safe space for individuals to share their experiences and connect with others going through similar situations.
By implementing these strategies and interventions, it is possible to manage symptoms and improve the quality of life for individuals living with pleural effusion and cancer.
Lifestyle Choices and Pleural Effusion Cancer Life Expectancy
Living with pleural effusion and cancer can be challenging, but making positive lifestyle choices can improve the prognosis and life expectancy of individuals with this condition.
One of the most important lifestyle choices is maintaining a healthy diet. Eating a balanced diet that is rich in fruits, vegetables, and whole grains can help the body fight cancer and support overall health. Additionally, limiting processed and high-fat foods can reduce the risk of developing other health complications.
Regular exercise is another essential factor in improving prognosis. Exercise can help strengthen the body, reduce fatigue, and improve mood. Research has shown that exercise is particularly effective in reducing the symptoms of pleural effusion, such as shortness of breath.
Refraining from smoking and excessive alcohol consumption can also improve outcomes and quality of life. These habits can worsen pleural effusion and cancer symptoms while placing additional strain on the body.
Managing stress and prioritizing mental health are crucial in coping with pleural effusion and cancer. Emotional support from family, friends, or mental health professionals can help individuals better manage stress. Engaging in mindfulness and relaxation techniques, such as yoga and meditation, can also improve well-being.
Incorporating healthy habits into daily life can increase life expectancy and improve the overall quality of life for individuals with pleural effusion and cancer. By taking care of oneself, it is possible to increase the chances of beating the disease and enjoying a fulfilling life.
Seeking Emotional Support for Pleural Effusion Cancer Patients and Caregivers
Dealing with pleural effusion and cancer can be emotionally challenging for both patients and caregivers. It is essential to seek support and find ways to cope with the stress and anxiety that can come with a cancer diagnosis.
Emotional Support Resources
There are various resources available to individuals seeking emotional support during this time. Support groups, therapy, and counseling services can provide helpful outlets for individuals to share their feelings and connect with others going through similar experiences. Online forums and support groups can also be valuable resources, especially for those who may not have access to in-person services or prefer the convenience of virtual support.
Caregiver Support
Caring for a loved one with pleural effusion and cancer can be both physically and emotionally demanding. Caregivers need to prioritize self-care and seek support when needed. Support groups and counseling services can provide a space for caregivers to share their experiences and discuss the challenges of caring for a loved one with cancer.
Self-Care Strategies
In addition to seeking emotional support, individuals with pleural effusion and cancer can benefit from self-care strategies that promote physical and emotional well-being. Exercise, meditation, and relaxation techniques can help reduce stress and promote a sense of calm. Engaging in enjoyable activities and connecting with loved ones can also provide a much-needed break from the demands of cancer treatment.
Remember, seeking emotional support is a sign of strength, not weakness. It is essential to find ways to cope with the emotional challenges of pleural effusion and cancer to promote overall well-being and improve quality of life.
Looking Towards the Future: Advances in Pleural Effusion Cancer Research
As medical research continues to progress, there is hope that new advances will be made in the diagnosis and treatment of pleural effusion in cancer patients.
One area of research that shows particular promise is in the use of immunotherapy. This treatment approach harnesses the body’s natural immune response to target and attack cancer cells. Preliminary studies have shown that immunotherapy can be effective in treating certain types of cancer, and researchers are now exploring its potential for managing pleural effusion in cancer patients.
Another area of interest is in the development of targeted therapies. These drugs are designed to specifically target cancer cells without harming healthy tissue, which can improve treatment outcomes and quality of life for patients. Some early-stage trials have shown promising results in using targeted therapies to manage pleural effusion in cancer patients.
Researchers are also exploring the use of gene therapy, which involves altering a patient’s genetic makeup to fight cancer cells. While still in the experimental stages, gene therapy has shown some potential for treating certain types of cancer, and may one day be a viable option for those with pleural effusion.
Overall, the future of pleural effusion cancer research is promising. New advances in technology and treatment approaches are constantly being discovered, and as such, the outlook for patients living with this condition is steadily improving.
FAQ
What is pleural effusion?
Pleural effusion is the buildup of fluid in the pleural cavity, the space between the lungs and the chest wall. It can occur as a complication of cancer and other medical conditions.
How is pleural effusion diagnosed?
Pleural effusion can be diagnosed through various imaging tests such as chest X-rays, CT scans, and ultrasound. A thoracentesis, a procedure to extract fluid from the pleural cavity, may also be performed for diagnosis.
What impact does pleural effusion have on cancer prognosis?
Pleural effusion can significantly affect the prognosis of cancer patients. The presence of pleural effusion often indicates advanced disease and can limit treatment options, potentially influencing life expectancy.
What are the factors that can influence life expectancy in individuals with pleural effusion and cancer?
Several factors can influence life expectancy, including the stage and type of cancer, the extent of pleural effusion, the overall health of the patient, and the response to treatment.
What are the treatment options for pleural effusion in cancer patients?
Treatment options for pleural effusion in cancer patients may include drainage procedures, such as thoracentesis or pleurodesis, chemotherapy, radiation therapy, and surgery to remove the tumor causing the effusion.
How do different treatment approaches impact life expectancy in pleural effusion cancer patients?
The impact of treatment on life expectancy varies depending on factors such as the stage and type of cancer, the response to treatment, and the overall health of the patient. It is important to discuss treatment options and their potential impact on prognosis with a healthcare provider.
What can be done to manage symptoms and improve the quality of life in pleural effusion cancer patients?
Strategies for managing symptoms and improving quality of life may include palliative care, pain management, and supportive therapies. Working closely with healthcare providers and seeking emotional support can also play a significant role.
How do lifestyle choices affect the life expectancy of individuals with pleural effusion and cancer?
Making healthy lifestyle choices, such as maintaining a balanced diet, engaging in regular exercise, and avoiding tobacco and excessive alcohol consumption, can positively impact the life expectancy of individuals with pleural effusion and cancer.
Where can individuals and caregivers seek emotional support for pleural effusion and cancer?
Seeking emotional support is crucial for both patients and caregivers. Support can be found through support groups, counseling services, and online communities dedicated to cancer and pleural effusion.
What are some advances in pleural effusion cancer research?
Ongoing research is focused on discovering new treatment approaches, improving diagnostic techniques, and finding targeted therapies for pleural effusion in cancer patients. These advancements have the potential to improve outcomes and life expectancy.