What to Expect After Lung Cancer Surgery – Recovering from lung cancer surgery can feel like a daunting journey. But knowing what lies ahead can make the process smoother and less overwhelming. Let’s break it down, step by step, so you know exactly what to expect and how to prepare.
What Happens During Lung Cancer Surgery?
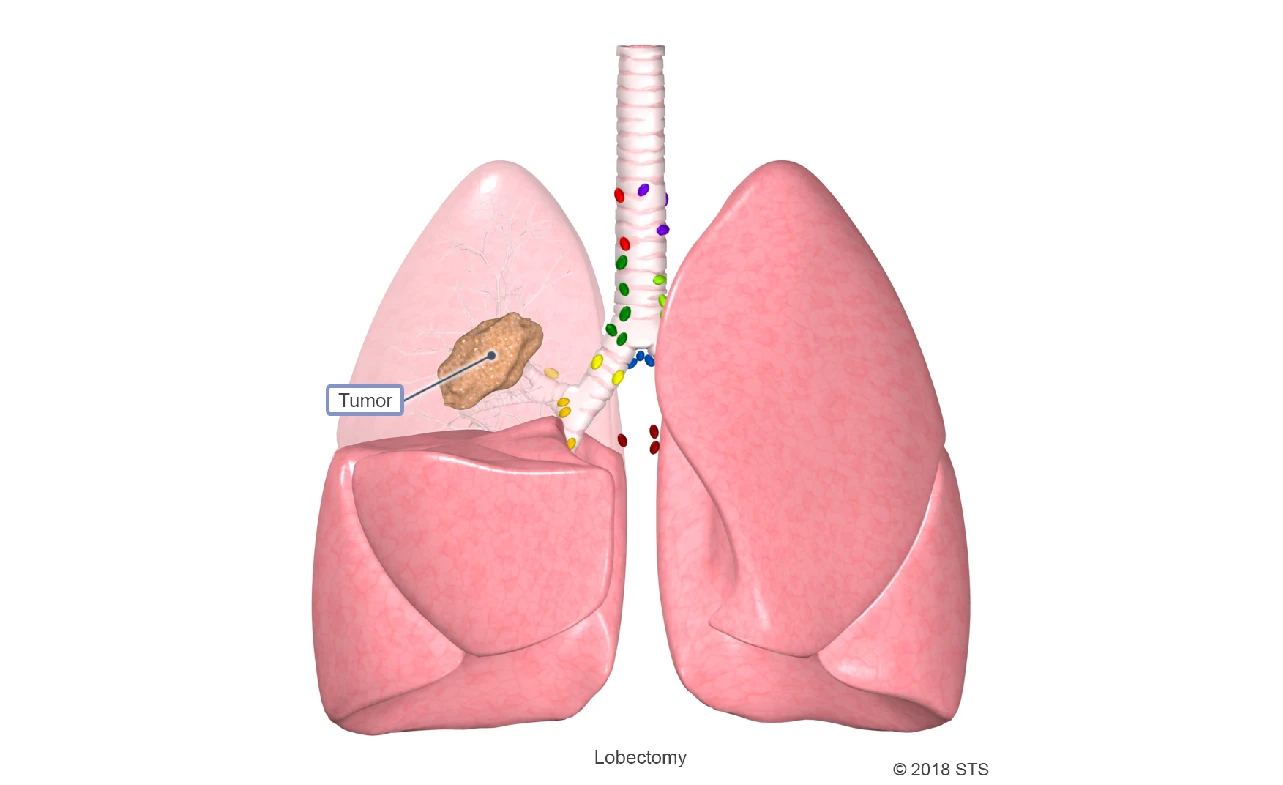
Lung cancer surgery typically involves removing a portion of the lung (lobectomy) or, in some cases, the entire lung (pneumonectomy). The specific procedure depends on the size, type, and location of the tumor. It’s usually performed under general anesthesia and can take several hours.
The primary goal? To remove cancerous tissue and give you the best chance at recovery. It’s a significant procedure, but understanding the basics can help you feel more in control.
Immediate Post-Surgery Recovery
Hospital Stay
Expect to stay in the hospital for 3-7 days, depending on the complexity of your surgery. Here’s what usually happens:
- Monitoring: Nurses and doctors will monitor your vitals and oxygen levels.
- Drainage Tubes: You might have tubes in your chest to drain fluid and air, which will be removed once your lungs heal sufficiently.
- Walking: Yes, they’ll encourage you to walk early on—even the day after surgery—to prevent blood clots and improve lung function.
What You’ll Feel
- Pain: It’s normal to experience pain near the incision site or in your chest.
- Fatigue: Surgery takes a toll on your body, so don’t be surprised if you feel drained.
Managing Pain and Discomfort
Pain management is a key part of recovery. Your doctor will prescribe medication to help you stay comfortable. Common options include:
- Prescription Painkillers: Stronger meds for immediate relief.
- Over-the-Counter (OTC) Pain Relievers: For milder discomfort.
- Nerve Blocks: Long-lasting pain relief injected near the surgical site.
Pro Tip: Don’t tough it out. Managing pain effectively helps you breathe deeper and move more, speeding up recovery.
Tips for Faster Healing
1. Focus on Breathing Exercises
Breathing exercises are crucial to regaining lung function. Your care team might give you an incentive spirometer—a small device to help you practice deep breathing.
2. Stay Active
While rest is important, gentle activities like walking can boost circulation, prevent clots, and help you bounce back faster.
3. Eat a Nutritious Diet
Fuel your body with:
- Protein-rich foods for tissue repair.
- Fruits and veggies for vitamins and antioxidants.
- Plenty of water to stay hydrated.
| Nutrient | Best Sources | Benefits |
|---|---|---|
| Protein | Chicken, fish, beans | Aids in tissue healing |
| Vitamin C | Oranges, strawberries | Strengthens the immune system |
| Iron | Spinach, red meat | Promotes oxygen delivery |
4. Follow Your Doctor’s Instructions
If they say no heavy lifting for six weeks, listen. Pushing your body too hard can set you back.
Emotional and Mental Recovery
Recovering from surgery isn’t just about physical healing; it’s a mental and emotional journey too. Many people feel anxious or even depressed after a major surgery. Here’s how to cope:
- Talk It Out: Share your feelings with loved ones or a counselor.
- Join a Support Group: Connecting with others who’ve been through the same experience can be incredibly comforting.
- Practice Mindfulness: Meditation and deep breathing can reduce stress and promote relaxation.
FAQs About Recovery
1. How long does full recovery take?
Recovery varies from person to person but generally takes 6-8 weeks for most activities. Full recovery can take up to 6 months.
2. Will I have a scar?
Yes, you’ll have a scar at the incision site, but it will fade over time. Ask your doctor about scar care options.
3. Can I drive after surgery?
Not immediately. Once you’re off pain meds and feel comfortable turning your body, driving is usually fine—typically after 2-3 weeks.
4. Is shortness of breath normal?
Yes, especially after exertion. It’s part of adjusting to reduced lung capacity, and it should improve over time.
Conclusion
Recovering from lung cancer surgery is a journey that requires patience, care, and support. From managing pain to focusing on emotional well-being, each step brings you closer to regaining your strength and returning to your routine.
Remember, every recovery is unique. Be kind to yourself, follow your doctor’s advice, and lean on your support system. Before you know it, you’ll be breathing easier and feeling stronger than ever.
Read more:
- Mutations in Lung Cancer” href=”https://www.haritravel.id/epidermal-growth-factor-receptor-mutations-in-lung-cancer/” rel=”bookmark”>Epidermal Growth Factor Receptor Mutations in Lung Cancer
- Understanding Stage 2 Lung Cancer Treatment
- Stage 4 Stomach Cancer Life Expectancy Without Treatment
- Stage 4 Cancer Life Expectancy Without Treatment
- Inoperable Lung Cancer Life Expectancy – Understanding Your Prognosis