Bone cancer melanoma is a rare but serious medical condition that often raises many questions among patients and their families. While melanoma is most commonly associated with the skin, in some cases it can spread to the bones, creating complications that require timely diagnosis and treatment. This condition can significantly affect a patient’s quality of life, making it important to understand the nature of the disease.
Learning about bone cancer melanoma, including its symptoms, causes, and treatment options, can help individuals take informed steps toward better health outcomes. By exploring medical insights, research advancements, and patient support resources, this article aims to provide a well-rounded overview of what to expect and how to manage the condition effectively.
Definition and Overview
Bone cancer melanoma refers to a form of melanoma that has spread from its original site, typically the skin, to the bones. This process is known as metastasis. Unlike primary bone cancer, which starts in the bone itself, melanoma that reaches the bones is considered metastatic cancer. It can weaken the skeletal structure and increase the risk of fractures.
This condition is relatively uncommon but often signals an advanced stage of melanoma. Because bones are essential for mobility, strength, and protection of internal organs, the spread of melanoma to this area can complicate treatment and require specialized care.
Types
Bone cancer melanoma may present in different forms depending on how the cancer spreads and which bones are affected:
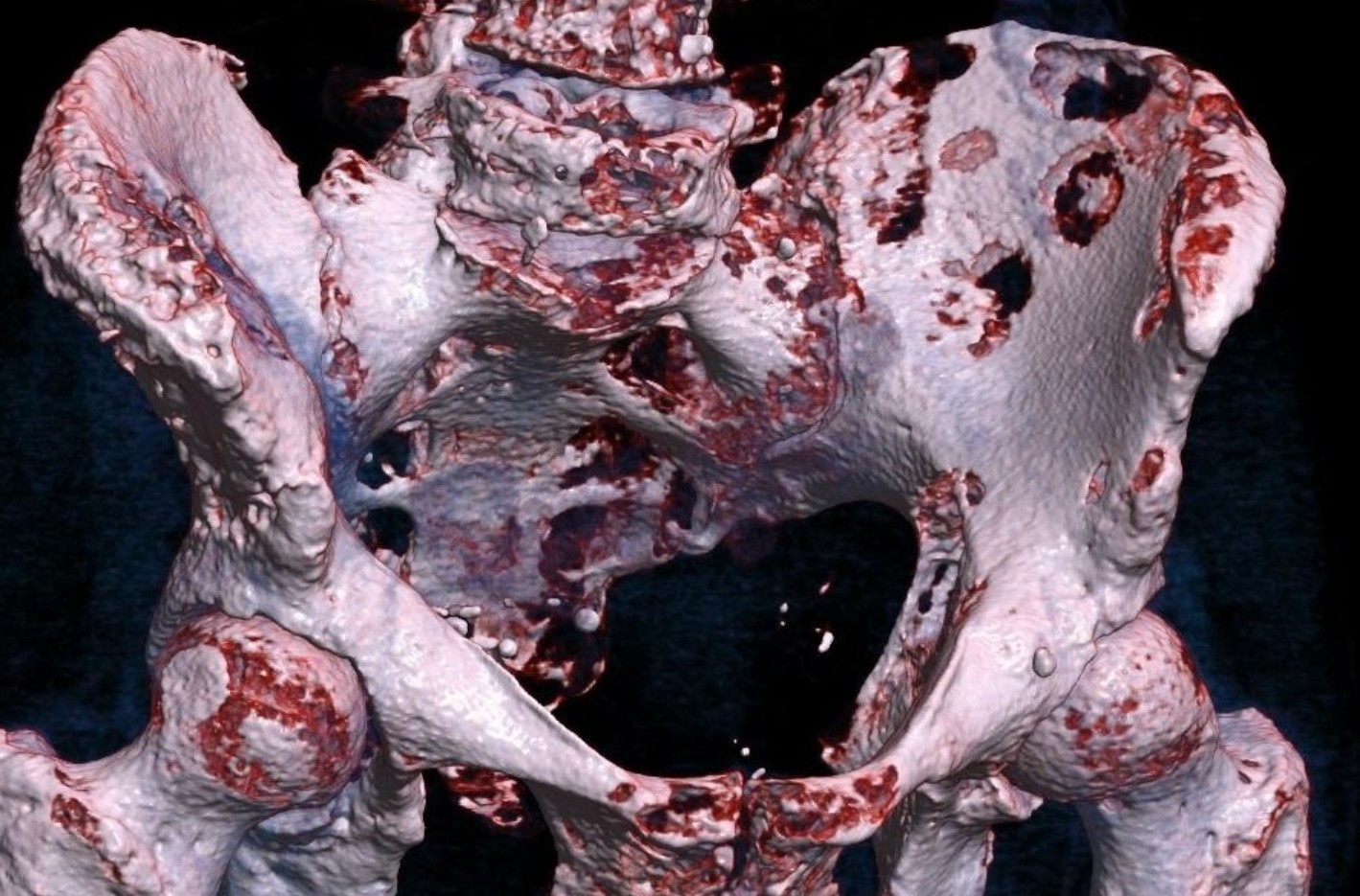
- Axial Bone Involvement – Melanoma that spreads to the spine, pelvis, or ribs.
- Appendicular Bone Involvement – Affects the arms or legs, leading to mobility issues.
- Diffuse Bone Metastasis – Cancer cells spread across multiple bones simultaneously.
- Localized Bone Metastasis – Melanoma cells are confined to one or two bones.
Each type requires tailored diagnostic methods and treatment strategies to ensure the best possible outcomes.
Causes and Risk Factors
Bone cancer melanoma develops when melanoma cells from the skin travel through the bloodstream or lymphatic system to the bones. Factors that increase the risk include:
- Advanced Stage Melanoma – Late detection often increases the chance of metastasis.
- Weakened Immune System – Patients with compromised immunity are more vulnerable.
- Genetic Predisposition – Family history of aggressive melanoma may play a role.
- Previous Cancer History – Prior melanoma increases the risk of recurrence in the bones.
Environmental and lifestyle factors, such as prolonged UV exposure, may indirectly contribute by increasing the likelihood of initial melanoma development.
Symptoms and Early Warning Signs
Recognizing the symptoms of bone cancer melanoma can lead to earlier intervention. Common signs include:
- Persistent bone pain, especially at night or during activity
- Swelling or tenderness near affected bones
- Increased risk of fractures from minor injuries
- Fatigue and unexplained weight loss
- Reduced mobility or stiffness in affected joints
Early detection can make a significant difference in treatment success and quality of life.
Diagnosis
Diagnosing bone cancer melanoma involves multiple steps to confirm the presence and extent of metastasis:
- Imaging Tests – X-rays, MRI, CT scans, and bone scans to detect affected areas.
- Biopsy – Tissue sample taken to confirm melanoma cells within the bone.
- Blood Tests – May reveal elevated levels of certain markers associated with cancer.
- PET Scans – Provide detailed insights into cancer spread throughout the body.
Accurate diagnosis helps doctors develop a personalized treatment plan for each patient.
Treatment Options
Treatment for bone cancer melanoma typically combines several approaches:
- Surgery – Removal of affected bone tissue or stabilization of fractures.
- Radiation Therapy – Used to reduce pain and control tumor growth.
- Chemotherapy – Targets rapidly dividing melanoma cells.
- Targeted Therapy – Drugs designed to attack specific cancer cell mutations.
- Immunotherapy – Boosts the body’s immune system to fight melanoma cells.
- Palliative Care – Focuses on relieving symptoms and improving quality of life.
A multidisciplinary team often manages the condition, ensuring patients receive both medical and supportive care.
Prevention and Lifestyle Recommendations
While it may not be possible to prevent bone cancer melanoma entirely, certain steps can reduce risks:
- Protect skin from excessive UV exposure to lower melanoma risk.
- Attend regular skin checks and screenings, especially if at high risk.
- Follow a balanced diet rich in antioxidants to support immune health.
- Stay physically active to maintain bone strength and mobility.
- Avoid smoking and excessive alcohol consumption, which can weaken overall health.
Early detection of melanoma and proactive management can significantly reduce the risk of it spreading to bones.
Prognosis and Survival Rates
The prognosis for bone cancer melanoma varies depending on factors such as the stage of melanoma, overall health, and how well the cancer responds to treatment. In general, melanoma that has spread to bones indicates an advanced stage, which can lower survival rates compared to early-stage melanoma.
However, medical advancements in immunotherapy and targeted therapies have improved outcomes for many patients. Continuous monitoring and follow-up care play a crucial role in extending survival and enhancing quality of life.
Latest Research and Innovations
Ongoing research continues to improve understanding and treatment of bone cancer melanoma. Some recent innovations include:
- Development of more effective immunotherapies targeting melanoma cells.
- Genetic testing to identify mutations and personalize treatment.
- Novel drug combinations to reduce resistance and enhance results.
- Advanced imaging techniques for earlier detection of bone metastasis.
These advancements provide hope for patients and families navigating this challenging condition.
Coping and Support for Patients
Living with bone cancer melanoma can be physically and emotionally demanding. Patients are encouraged to seek support from:
- Counseling Services – To help manage anxiety and emotional stress.
- Support Groups – Connecting with others facing similar challenges.
- Rehabilitation Programs – Assisting with mobility and daily activities.
- Family and Caregiver Support – Strengthening emotional and practical resources.
A strong support system can make a meaningful difference in treatment adherence and overall well-being.
Conclusion
Bone cancer melanoma is a serious condition that requires timely medical attention, comprehensive treatment, and ongoing support. Understanding its causes, symptoms, and available therapies can empower patients and families to make informed healthcare decisions.
While the prognosis can be challenging, modern medical research and innovative treatments offer new possibilities for improved outcomes. By staying informed and proactive, patients can navigate bone cancer melanoma with greater confidence and hope.