Prostate cancer is one of the most common cancers among men worldwide, making early detection and proper documentation essential for effective treatment and healthcare management. To standardize the classification and coding of medical conditions, physicians and hospitals rely on the ICD 10 for prostate cancer. This coding system not only supports accurate diagnosis but also helps in healthcare billing, insurance claims, and statistical analysis of cancer prevalence.
Understanding the ICD 10 for prostate cancer is crucial for both healthcare providers and patients. By knowing what each code represents, medical professionals can ensure precise medical records, while patients can gain a clearer view of their condition. In this article, we will explore the definition, types, risk factors, symptoms, diagnostic methods, treatments, and the latest research, providing a comprehensive guide to navigating prostate cancer and its coding system.
Definition and Overview
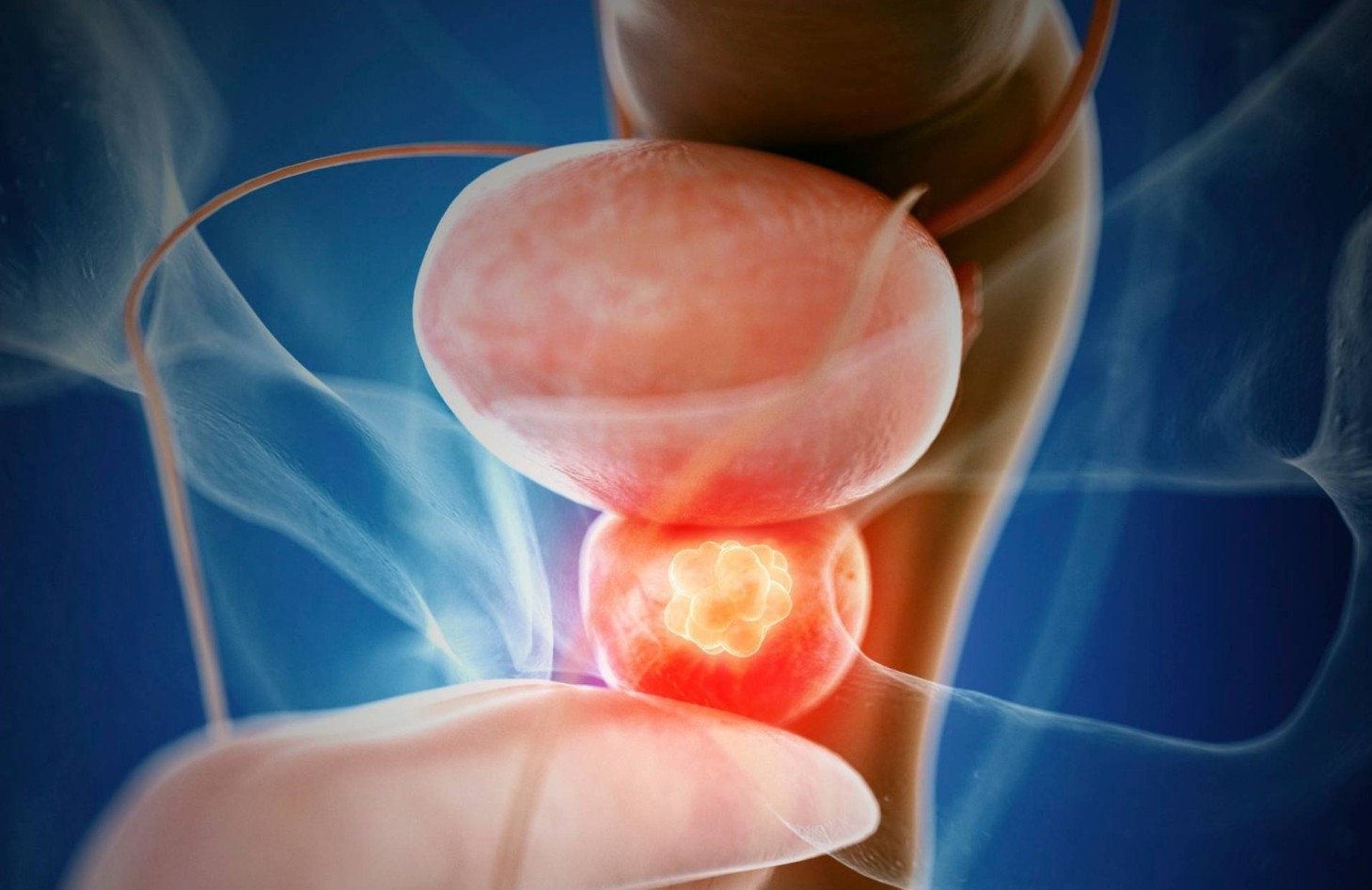
The ICD 10 for prostate cancer refers to a specific coding system used by the International Classification of Diseases, 10th Revision (ICD-10), which categorizes prostate cancer under the code C61. This classification ensures uniformity in identifying, reporting, and tracking prostate cancer cases globally. Prostate cancer develops in the prostate gland, a small walnut-shaped organ in men that produces seminal fluid essential for reproduction.
By using ICD 10 coding, healthcare providers can streamline documentation, enhance treatment planning, and contribute to worldwide cancer research. The coding system plays a vital role not only in diagnosis but also in health insurance processes and epidemiological studies.
Types
Prostate cancer can manifest in different forms, and the ICD 10 for prostate cancer encompasses these variations. The primary types include:
- Adenocarcinoma of the prostate: The most common type, originating from glandular cells.
- Small cell carcinoma: A rare and aggressive form.
- Squamous cell carcinoma: Extremely rare and typically more resistant to treatment.
- Transitional cell carcinoma: Usually starts in the bladder and spreads to the prostate.
Recognizing the type of cancer is crucial, as it influences both prognosis and treatment strategy.
Causes and Risk Factors
Although the exact cause of prostate cancer remains unclear, several factors increase the likelihood of developing it. Common risk factors include:
- Age: Men over 50 are at greater risk.
- Family history: Genetic predisposition plays a significant role.
- Ethnicity: African American men are more likely to develop aggressive forms.
- Diet and lifestyle: High-fat diets and obesity can contribute to risk.
- Hormonal factors: Elevated testosterone levels may influence cancer growth.
Understanding these factors allows individuals to adopt preventive measures and monitor their health more closely.
Symptoms and Early Warning Signs
Early stages of prostate cancer often show no symptoms, making regular screenings vital. As the disease progresses, common symptoms may include:
- Difficulty urinating or weak urine flow
- Frequent urination, especially at night
- Blood in urine or semen
- Erectile dysfunction
- Pain in the hips, back, or chest (in advanced cases)
Recognizing these warning signs early can lead to quicker diagnosis and more effective treatment.
Diagnosis
Accurate diagnosis is essential for proper treatment planning. The process often involves multiple tests, including:
- Prostate-Specific Antigen (PSA) test: Measures PSA levels in the blood.
- Digital Rectal Exam (DRE): Detects abnormalities in the prostate gland.
- Biopsy: Confirms cancer by analyzing tissue samples.
- Imaging tests: MRI, CT scans, or bone scans to detect cancer spread.
Each diagnosis is documented using the ICD 10 for prostate cancer, ensuring consistency across healthcare systems.
Treatment Options
Treatment depends on the stage, type, and patient health condition. Common treatment methods include:
- Active surveillance: Monitoring cancer in early stages without immediate treatment.
- Surgery (prostatectomy): Removal of the prostate gland.
- Radiation therapy: Targeted radiation to kill cancer cells.
- Hormone therapy: Reducing testosterone to slow cancer growth.
- Chemotherapy: Used in advanced or aggressive cases.
- Immunotherapy: Boosts the body’s immune system to fight cancer.
Each approach has its benefits and potential side effects, so treatment plans must be tailored to each patient.
Prevention and Lifestyle Recommendations
While prostate cancer cannot always be prevented, certain lifestyle changes can lower risks:
- Eating a balanced diet rich in fruits, vegetables, and lean proteins
- Reducing intake of red meat and high-fat foods
- Maintaining a healthy weight and exercising regularly
- Limiting alcohol consumption and avoiding smoking
- Undergoing regular check-ups and PSA screenings
These habits support overall health and may reduce the likelihood of developing prostate cancer.
Prognosis and Survival Rates
The prognosis for prostate cancer largely depends on how early it is detected. When diagnosed in the localized stage, the survival rate is very high, often exceeding 90%. However, advanced cases that spread to other organs may lower survival outcomes. Thanks to advances in medical research and treatment, many men live long and healthy lives after a prostate cancer diagnosis.
Latest Research and Innovations
Medical research continues to improve the outlook for patients. Current innovations include:
- Precision medicine: Tailoring treatments based on genetic profiles.
- Advanced imaging techniques: Improving early detection and monitoring.
- New drug therapies: Offering better outcomes for resistant cancers.
- Robotic-assisted surgery: Enhancing precision with fewer complications.
These innovations, combined with the standardized use of the ICD 10 for prostate cancer, ensure more effective and personalized treatment approaches.
Coping and Support for Patients
A prostate cancer diagnosis can be emotionally and physically challenging. Patients benefit from support systems such as:
- Counseling and mental health services
- Support groups with fellow survivors
- Nutritional guidance for healthier recovery
- Family and caregiver involvement
- Educational resources about managing side effects
Emotional resilience and community support are just as important as medical treatment in coping with prostate cancer.
Conclusion
Understanding the ICD 10 for prostate cancer is not just about medical coding—it is about ensuring accurate diagnosis, effective treatment, and better healthcare outcomes for patients worldwide. By recognizing symptoms early, adopting preventive lifestyles, and leveraging the latest research, men can significantly improve their chances of recovery.
As medical science advances, the combination of standardized ICD 10 coding and innovative treatment methods will continue to enhance the quality of care for prostate cancer patients. Staying informed and proactive remains the key to managing this condition successfully.