Facing pancreatic and liver cancer final stages can be an overwhelming experience for both patients and their loved ones. These advanced phases of cancer often bring significant physical, emotional, and medical challenges. Understanding what happens during these stages is crucial to making informed decisions about care, treatment, and overall quality of life.
While each patient’s journey is unique, the final stages of pancreatic and liver cancer tend to share similar symptoms and patterns. This article provides a comprehensive overview, from definitions and risk factors to diagnosis, treatment approaches, and supportive care. It also highlights recent research and ways families can cope during these difficult times.
Definition and Overview
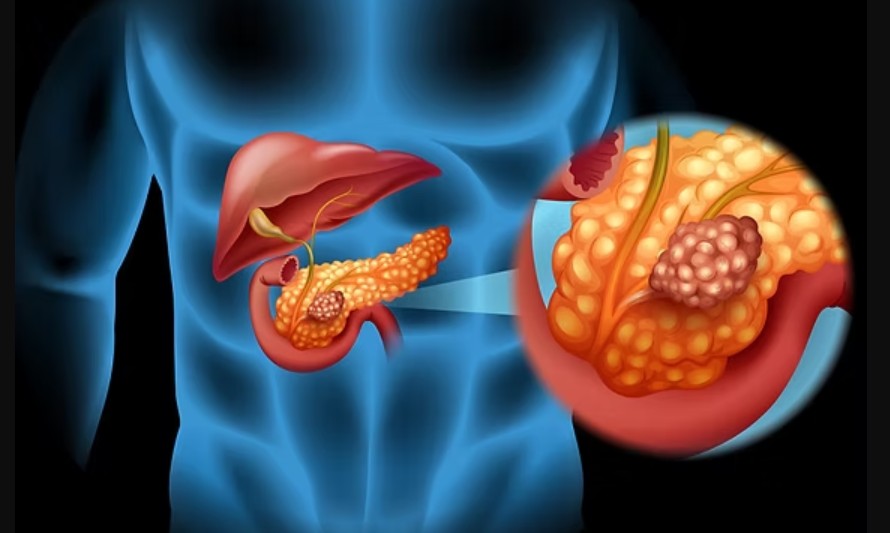
Pancreatic cancer originates in the pancreas, an organ responsible for producing enzymes and hormones like insulin. Liver cancer, on the other hand, develops in the liver, which plays a central role in detoxifying the blood, storing nutrients, and supporting digestion. When these cancers progress to their final stages, the disease has usually spread extensively, making curative treatment unlikely.
The final stages of pancreatic and liver cancer are typically categorized as stage IV. This means the cancer has metastasized to distant organs, significantly impairing bodily functions. At this point, treatment goals shift primarily toward palliative care, aiming to relieve symptoms and maximize comfort.
Types
Pancreatic Cancer Types
- Exocrine tumors: The most common form, accounting for over 90% of pancreatic cancers.
- Endocrine tumors: Rare tumors affecting hormone-producing cells.
Liver Cancer Types
- Hepatocellular carcinoma (HCC): The most common type, often linked to chronic liver disease.
- Intrahepatic cholangiocarcinoma: A rarer form affecting bile ducts within the liver.
- Secondary liver cancer: Cancer that spreads (metastasizes) to the liver from another organ.
Causes and Risk Factors
Several factors increase the likelihood of developing pancreatic or liver cancer. These include:
- Genetic predisposition: Family history and inherited mutations.
- Chronic conditions: Such as pancreatitis, cirrhosis, or hepatitis B and C.
- Lifestyle habits: Smoking, excessive alcohol use, and high-fat diets.
- Obesity and diabetes: Both conditions elevate cancer risk.
- Environmental exposures: Contact with harmful chemicals or toxins.
In the final stages of pancreatic and liver cancer, these risk factors have typically contributed to long-term damage, accelerating disease progression.
Symptoms and Early Warning Signs
Common Symptoms in Final Stages
- Severe abdominal pain or back pain
- Unintentional weight loss and extreme fatigue
- Jaundice (yellowing of the skin and eyes)
- Loss of appetite and digestive problems
- Fluid buildup in the abdomen (ascites)
- Nausea, vomiting, and difficulty eating
- Mental confusion or changes in behavior
Recognizing these symptoms can help families prepare and seek timely medical or palliative care.
Diagnosis
Diagnosis of pancreatic and liver cancer final stages involves a combination of:
- Imaging tests: CT scans, MRI, PET scans, and ultrasounds to assess tumor spread.
- Blood tests: Checking for tumor markers such as CA 19-9 for pancreatic cancer and AFP for liver cancer.
- Biopsy: Collecting tissue samples to confirm the cancer type.
- Physical examination: Identifying jaundice, abdominal swelling, or weight loss.
In late stages, diagnosis often focuses more on symptom management rather than curative treatment planning.
Treatment Options
Treatment in the final stages typically emphasizes comfort and symptom relief. Options may include:
- Palliative chemotherapy or radiation: To slow cancer growth and relieve pain.
- Targeted therapy: For patients eligible based on genetic testing.
- Pain management: Opioids and nerve blocks to control severe discomfort.
- Nutritional support: Ensuring patients receive adequate hydration and energy.
- Hospice care: Providing comprehensive support for patients nearing end of life.
Prevention and Lifestyle Recommendations
While prevention may not help during the final stages, it plays a crucial role earlier in life. Key recommendations include:
- Avoid smoking and limit alcohol consumption.
- Maintain a healthy weight and balanced diet.
- Get vaccinated against hepatitis B.
- Undergo regular health screenings, especially if at high risk.
- Manage underlying conditions like diabetes and liver disease.
Prognosis and Survival Rates
The prognosis for pancreatic and liver cancer final stages is generally poor. Pancreatic cancer has a five-year survival rate of less than 10%, and liver cancer survival rates are also low in advanced stages. Once the disease reaches stage IV, life expectancy is often measured in months rather than years.
However, supportive care can make a significant difference in quality of life. Every patient responds differently, and compassionate care remains essential.
Latest Research and Innovations
Research into pancreatic and liver cancer is ongoing, with promising areas including:
- Immunotherapy: Boosting the body’s immune system to target cancer cells.
- Personalized medicine: Tailoring treatments based on genetic testing.
- New imaging technologies: Helping detect cancer earlier and track treatment response.
- Novel drug therapies: Investigating agents that may slow tumor progression.
Although these advances may not always benefit patients in the final stages, they offer hope for future generations.
Coping and Support for Patients
Coping with the final stages of pancreatic and liver cancer requires strong emotional and psychological support. Patients and families often benefit from:
- Counseling and therapy: To manage emotional distress.
- Support groups: Sharing experiences with others facing similar challenges.
- Spiritual care: For those seeking comfort through faith or belief systems.
- Caregiver support: Training and resources for family members providing daily care.
Emphasizing dignity, comfort, and meaningful connections is vital during this difficult time.
Conclusion
The journey through pancreatic and liver cancer final stages is undoubtedly challenging, but understanding the disease helps patients and families prepare with clarity and compassion. From recognizing symptoms to exploring palliative care options, awareness empowers better decision-making.
Although survival rates are limited in advanced stages, ongoing research and supportive care provide hope and comfort. By focusing on quality of life, meaningful relationships, and emotional well-being, patients and their loved ones can face this chapter with strength and resilience.