Stagescancer.net – Stage 3 liver cancer is a serious diagnosis, with a significant impact on life expectancy. In this section, we will explore important factors that can influence the prognosis of patients diagnosed with stage 3 liver cancer. According to the American Cancer Society, the five-year survival rate for stage 3 liver cancer is around 22%. However, many factors can impact this estimate, and patients are urged to speak with their healthcare provider to understand their individual prognosis.
Some of the factors influencing life expectancy for those with stage 3 liver cancer include the size and number of tumors, involvement of nearby lymph nodes, and the extent of the cancer’s spread. Additionally, age, overall health, response to treatment, and the presence of underlying health conditions can all play a role in determining life expectancy.
In the following sections, we will explore the different treatments available for stage 3 liver cancer and their effectiveness in improving life expectancy. We will also discuss coping strategies for patients and families, the role of palliative care and hospice services, and the promising research and clinical trials currently underway in this field.
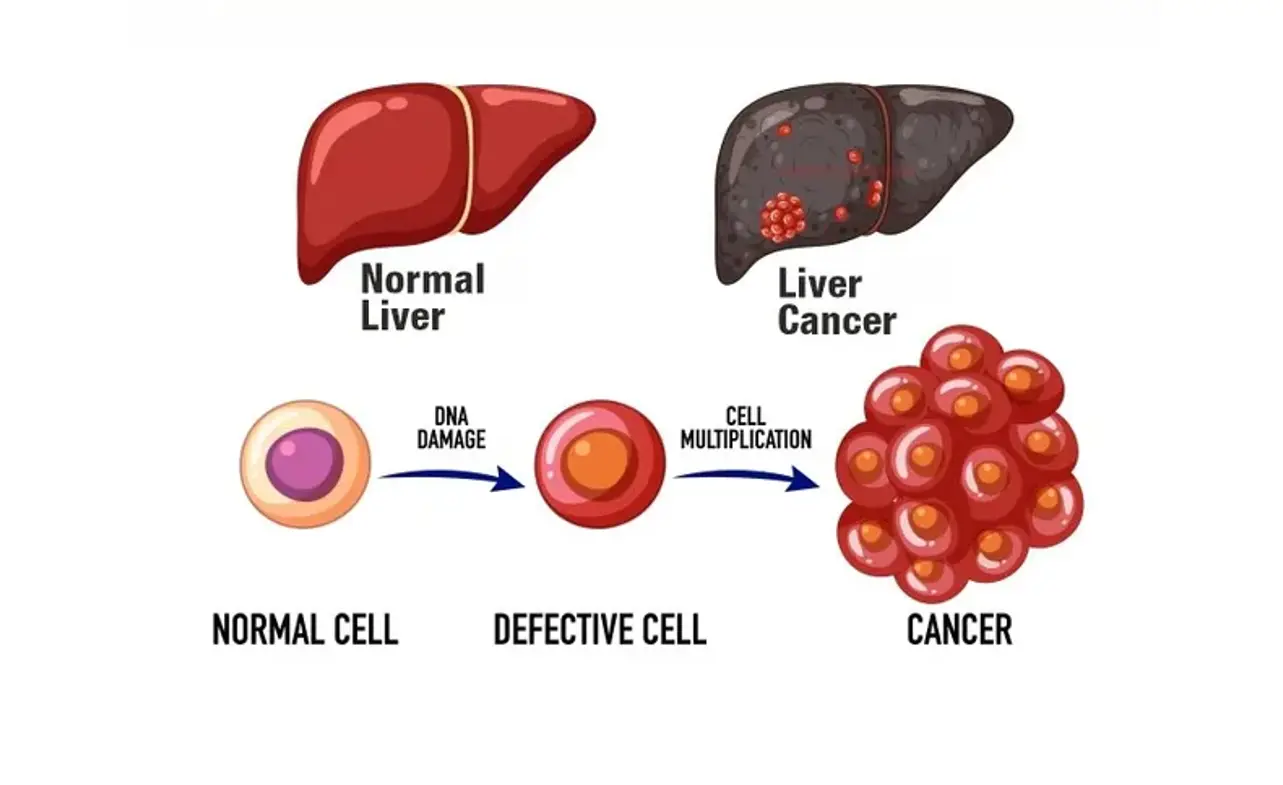
Understanding Stage 3 Liver Cancer
Stage 3 liver cancer is a form of cancer that often affects older adults and typically occurs when cancer spreads to nearby tissues and lymph nodes. Symptoms of stage 3 liver cancer may include abdominal pain, weight loss, fatigue, and jaundice. Diagnosing stage 3 liver cancer often involves imaging tests, such as CT scans, MRIs, and PET scans, as well as blood tests and biopsies.
It is essential to understand the nature of stage 3 liver cancer to determine the most effective treatment options and predict life expectancy. Stage 3 liver cancer is a complex condition that requires a multidisciplinary approach involving medical professionals in various specialties, including medical and surgical oncology, radiology, and gastroenterology.
While liver cancer can be challenging to treat, there are numerous treatment options available that can significantly improve patient outcomes.
Prognosis of Stage 3 Liver Cancer
After diagnosis of stage 3 liver cancer, patients are naturally curious about their prognosis. Unfortunately, the prognosis for stage 3 liver cancer is generally poor compared to earlier stages of the disease.
However, the exact prognosis will depend on a wide range of factors. These may include the size and number of tumors, involvement of nearby lymph nodes, and the extent of the cancer’s spread.
According to recent studies, the overall 5-year survival rate for stage 3 liver cancer is around 22%. This means that only around 22% of people who receive a diagnosis of stage 3 liver cancer will survive for at least 5 years after their diagnosis.
Factors that Influence Prognosis
While the prognosis for stage 3 liver cancer is generally poor, there are some factors that can impact a patient’s individual prognosis.
- Cancer stage: As mentioned, the exact stage of the cancer at diagnosis will play a significant role in determining prognosis. Additionally, factors such as the size and number of tumors, and whether the cancer has spread to nearby organs or lymph nodes can also impact prognosis.
- Patient’s general health: Patients who are otherwise healthy and have a strong immune system may be better able to tolerate treatment and potentially improve their prognosis.
- Treatment response: How well a patient responds to treatment can also impact their prognosis. Patients who show a positive response to treatment may be more likely to survive longer than those who do not respond as well.
It is important to keep in mind that every patient’s prognosis will be unique to their individual situation and cannot be predicted with certainty.
Factors Influencing Life Expectancy
Life expectancy for individuals with stage 3 liver cancer can be influenced by a multitude of factors. One of the most significant factors is age. As a general rule, older individuals tend to have a shorter life expectancy due to their reduced ability to tolerate rigorous treatment regimes.
Other factors that can play a role in life expectancy include overall health, response to treatment, and the presence of underlying health conditions. Patients with pre-existing health conditions may have a reduced life expectancy due to the increased complexity of their case.
Response to Treatment
Response to treatment is often the most significant factor in determining life expectancy for individuals with stage 3 liver cancer. Patients who respond well to treatment and experience remission may have a significantly longer life expectancy than those who do not.
Another factor that can impact life expectancy is the specific type of treatment received. Further research is required to determine which treatments are most effective in prolonging life for individuals with stage 3 liver cancer, as the optimal treatment approach may vary depending on the individual.
Presence of Underlying Health Conditions
Patients with underlying health conditions may have a reduced life expectancy due to the increased complexity of their case. These health conditions may limit the patient’s ability to tolerate rigorous treatment regimes, or they may impact the effectiveness of treatment.
It is important for individuals with stage 3 liver cancer to work closely with their healthcare team to manage any underlying health conditions and maximize their chances of achieving remission.
Treatment Options for Stage 3 Liver Cancer
When it comes to treating stage 3 liver cancer, there are several options available. The choice of treatment will depend on several factors, including the size and location of the tumor, the number of tumors, and the overall health and preference of the patient. The main treatment options are:
- Surgical Interventions: Surgery is a common treatment option for stage 3 liver cancer. It involves removing the tumor or a part of the liver. The most commonly used surgical procedures are hepatectomy, liver transplant, and ablation techniques.
- Radiation Therapy: Radiation therapy uses high-energy radiation to target and destroy cancer cells. It may be used as a stand-alone treatment or in combination with other therapies to shrink tumors before surgery, reduce pain and symptoms, or eliminate remaining cancer cells after surgery.
- Chemotherapy: Chemotherapy treats stage 3 liver cancer with anti-cancer drugs. It can be given orally or through an IV, and works by killing rapidly dividing cancer cells. Combination chemotherapy, which uses different drugs, may be more effective than single-agent chemotherapy in advanced liver cancer cases.
- Targeted Therapy: Targeted therapy is a type of cancer treatment that targets specific proteins or genes that contribute to cancer growth. It can be used as a stand-alone therapy or in combination with other treatments such as chemotherapy or radiation. Several targeted therapy drugs are available for the treatment of advanced liver cancer.
- Immunotherapy: Immunotherapy uses the body’s immune system to fight cancer cells. It may be used as a stand-alone treatment or in combination with other therapies. Immunotherapy drugs that have been approved for the treatment of advanced liver cancer include nivolumab and pembrolizumab.
The choice of treatment for stage 3 liver cancer can be complex and should be based on a thorough evaluation of the patient’s condition and available treatment options. Consulting with healthcare professionals who specialize in liver cancer treatment can help patients make informed decisions about the most appropriate treatment approach for their specific case.
Surgery for Stage 3 Liver Cancer
When it comes to treating stage 3 liver cancer, surgery is an option that may be considered. There are several surgical approaches that may be taken, depending on the size, location, and extent of the tumor, as well as the overall health of the patient.
Resection: This surgical procedure involves the removal of the tumor and a portion of the liver tissue surrounding it. This approach is typically only considered if the tumor is small and localized in one area of the liver. The remaining portion of the liver can regenerate and regain function.
Liver Transplantation: This surgical procedure involves the removal of the entire liver and replacing it with a healthy liver from a donor. This approach is considered when the tumor is too large for resection or cancer has spread to nearby blood vessels.
| Surgery Type | Benefits | Risks |
|---|---|---|
| Resection | – The best chance for a cure – Shorter hospital stay |
– Risk of bleeding, infection, liver failure, or recurrence |
| Liver Transplantation | – Chance for prolonged survival – The remaining portion of the liver will regenerate and regain function |
– Risk of rejection – Finding a suitable donor can be difficult – Recurrence of cancer is possible |
| Ablation Techniques | – Minimal invasiveness – Shorter hospital stay |
– Not recommended for large tumors – Incomplete destruction of tumor cells is possible – Risk of complications such as bleeding, infection, or perforation of the bile duct |
Ablation Techniques: These minimally invasive procedures use heat or cold to destroy cancer cells. Ablation techniques may be used in some cases when patients are not eligible for surgery.
It is important to note that surgery may not be the best option for every patient with stage 3 liver cancer. The decision to undergo surgery should be based on several factors, including the overall health of the patient, the size and number of the tumors, and the extent of the cancer’s spread. Patients should discuss all treatment options with their healthcare providers to make an informed decision.
Radiation Therapy for Stage 3 Liver Cancer
Radiation therapy uses high-energy radiation to kill cancer cells and can be a useful treatment option for stage 3 liver cancer patients. It is often used in combination with other treatments, such as chemotherapy or surgery.
The most common type of radiation therapy used to treat liver cancer is external beam radiation therapy. This type of treatment uses a machine to deliver radiation directly to the cancerous tumors from outside the body. Another type of radiation therapy is called brachytherapy, in which small radioactive seeds are implanted into the liver tissue near the tumor.
While radiation therapy can be an effective treatment option, it may also cause side effects such as fatigue, nausea, and skin irritation. Additionally, it may not be suitable for all patients, especially those with extensive liver damage or tumors that are too large or too close to critical organs. Your doctor will consider various factors, including your general health and the stage of your cancer when deciding if radiation therapy is the right treatment option for you.
| Radiation Therapy for Stage 3 Liver Cancer | Pros | Cons |
|---|---|---|
| External Beam Radiation Therapy | – Non-invasive procedure – Effective in targeting cancer cells directly |
– Potential side effects such as fatigue, nausea, and skin irritation – May not be suitable for all patients |
| Brachytherapy | – Can deliver a higher dose of radiation to the tumor – Minimal radiation exposure to healthy tissue |
– Invasive procedure – Radiation exposure to healthcare workers participating in the implantation process |
If radiation therapy is recommended as part of your treatment plan, your medical team will provide you with detailed instructions on how to prepare for treatment and manage any side effects that may occur. They will also monitor your progress to ensure the treatment is effective.
Chemotherapy as a Treatment Option for Stage 3 Liver Cancer
Chemotherapy involves the use of drugs to destroy cancer cells in the body. It can be administered in various ways, such as orally, intravenously, or through an injection. Chemotherapy is one of the treatment options for stage 3 liver cancer that can help prolong life expectancy.
There are different types of chemotherapy drugs that can be used, either as a single agent or in combination with other drugs. Commonly used drugs include cisplatin, 5-fluorouracil, doxorubicin, and oxaliplatin. Chemotherapy can also be used in combination with other treatments such as surgery or radiation therapy.
While chemotherapy can be effective in treating stage 3 liver cancer, it can cause various side effects, such as hair loss, nausea, vomiting, and fatigue. The severity and type of side effects may vary depending on the drugs used and the patient’s general health condition.
Studies have shown that combination chemotherapy can improve the prognosis and survival rates of patients with stage 3 liver cancer. However, each patient’s response to chemotherapy may vary, and it is essential to discuss the potential risks and benefits with a healthcare provider.
Targeted Therapy for Stage 3 Liver Cancer
As an emerging treatment option, targeted therapy for stage 3 liver cancer is gaining attention due to its potential to selectively attack cancer cells while sparing healthy tissue. Targeted drugs work by blocking the specific molecules or receptors that contribute to the growth and survival of cancer cells.
Targeted therapy for stage 3 liver cancer may involve drugs such as sorafenib and lenvatinib, which are FDA-approved for use in advanced liver cancer. These drugs can inhibit the formation of new blood vessels that feed the tumor, thereby limiting its ability to grow and spread.
Potential Side Effects
While targeted therapy has shown promise in treating stage 3 liver cancer, it can also cause side effects. These may include fatigue, nausea, diarrhea, skin rashes, and elevated blood pressure. Some targeted drugs can also cause more severe side effects, such as potential liver damage.
Current Status of Research
Ongoing research is focused on developing new targeted drugs and improving the effectiveness of existing ones. Clinical trials are underway to evaluate the safety and efficacy of these drugs in combination with other treatment options, such as chemotherapy, immunotherapy, and radiation therapy.
| Treatment | Median Overall Survival (Months) | Median Time to Progression (Months) |
|---|---|---|
| Sorafenib | 10.7 | 5.5 |
| Lenvatinib | 13.6* | 7.4 |
*Lenvatinib plus pembrolizumab
As shown in the table, both sorafenib and lenvatinib have demonstrated a survival benefit in advanced liver cancer. Combination therapy involving lenvatinib and immunotherapy shows promise in improving response rates and overall survival.
Despite the potential benefits of targeted therapy, it is essential to consult with a healthcare team to determine the best treatment plan for individual patients.
Immunotherapy for Stage 3 Liver Cancer
Immunotherapy has emerged as a promising treatment option for stage 3 liver cancer. This approach works by stimulating the body’s immune system to target and destroy cancer cells.
There are different types of immunotherapy used in the treatment of stage 3 liver cancer, including checkpoint inhibitors, CAR T-cell therapy, and oncolytic virus therapy. Each approach has a unique mechanism of action and potential benefits.
Checkpoint Inhibitors
Checkpoint inhibitors are a type of immunotherapy that works by blocking certain proteins on immune cells, allowing them to effectively attack cancer cells. These drugs have shown promise in clinical trials for treating liver cancer.
| Checkpoint Inhibitors for Stage 3 Liver Cancer | Common Drugs | Mechanism of Action | Potential Side Effects |
|---|---|---|---|
| CTLA-4 Inhibitors | Tremelimumab | Blocks CTLA-4 protein, allowing immune cells to attack cancer cells | Fatigue, diarrhea, skin rash, liver problems |
| PD-1 Inhibitors | Nivolumab, Pembrolizumab | Blocks PD-1 protein, allowing immune cells to attack cancer cells | Fatigue, decreased appetite, nausea, diarrhea, skin rash |
CAR T-Cell Therapy
CAR T-cell therapy involves modifying a patient’s T-cells to specifically target cancer cells. This approach has shown promising results in clinical trials for treating liver cancer.
However, CAR T-cell therapy also carries a risk of severe side effects, such as cytokine release syndrome and neurotoxicity.
Oncolytic Virus Therapy
Oncolytic virus therapy is a type of immunotherapy that uses modified viruses to target and destroy cancer cells. This approach has shown potential in early clinical trials for liver cancer treatment.
Common oncolytic viruses used in clinical trials for liver cancer include the Seneca Valley virus, Coxsackievirus, and Vaccinia virus.
Despite the promise of immunotherapy, its effectiveness and safety for stage 3 liver cancer treatment are still being studied. However, these treatments offer hope and potential benefits for patients fighting the disease, and continued research in immunotherapy is underway.
Survival Rates for Stage 3 Liver Cancer
Stage 3 liver cancer is an aggressive disease, and survival rates vary depending on a variety of factors. According to the American Cancer Society, the overall 5-year survival rate for individuals with liver cancer is about 20%. However, it is important to note that survival rates for stage 3 liver cancer specifically are typically lower than this average.
Factors that can impact survival rates include the size and location of the tumors, whether the cancer has spread to nearby lymph nodes or other organs, and the overall health of the patient. The presence of underlying health conditions, such as hepatitis or cirrhosis, can also impact survival rates.
Advancements in treatment options have led to improved outcomes for some patients with stage 3 liver cancer. For example, the use of immunotherapy has shown promise in clinical trials and may provide a new avenue for treatment. However, further research is necessary to fully understand the potential of this approach.
| Group | Survival Rate |
|---|---|
| Overall | 5% |
| U.S. Patients with Surgery | 24% |
| U.S. Patients without Surgery | 7% |
It is important to note that survival rates are not a guarantee. Each individual’s situation is different, and survival rates cannot predict how long a person with stage 3 liver cancer will live. However, understanding the factors that influence survival rates can help patients and their loved ones make informed decisions about treatment options and prepare for the future.
Coping with Stage 3 Liver Cancer
Being diagnosed with stage 3 liver cancer can be overwhelming and stressful. Coping with the disease involves building a strong support network and taking care of your mental well-being. Connecting with loved ones, support groups, and counseling services can help alleviate feelings of isolation and anxiety.
It’s essential to prioritize self-care and seek out resources to help navigate the challenges of the disease. Exercise, relaxation techniques, and a balanced diet can play a significant role in supporting overall well-being. Additionally, staying informed about treatment options, managing symptoms, and staying organized with medical appointments and paperwork can help maintain a sense of control and reduce stress.
There are also a variety of resources available to individuals with stage 3 liver cancer and their families. The American Cancer Society, Liver Cancer Foundation, and CancerCare are excellent starting points for finding information and support. These resources can provide opportunities to connect with others facing similar challenges, get practical advice from experts, and access financial assistance programs.
Palliative Care and Hospice Services
When it comes to stage 3 liver cancer, medical treatment is not the only type of care that patients need. Palliative care and hospice services offer valuable support to patients and their loved ones during this difficult time.
Palliative care is focused on enhancing the quality of life for individuals with serious illnesses, including stage 3 liver cancer. It can be provided alongside curative treatments and aims to address the physical, emotional, and spiritual needs of patients. Palliative care can also help manage pain, address symptoms, and improve the overall comfort of patients.
Hospice services offer specialized care to patients with terminal illnesses, including stage 3 liver cancer. Hospice care is typically provided when curative treatments are no longer an option, and the focus shifts to comfort care. Hospice services aim to improve the quality of life for patients and their families, providing emotional, psychological, and spiritual support during end-of-life care.
Discussing palliative care and hospice services with healthcare providers can provide patients with a better understanding of what to expect and the options available to them. It is essential to take advantage of these resources as they can help to manage symptoms, improve overall well-being, and provide much-needed support to patients and their families.
Research and Future Perspectives
Despite the progress made in the treatment of stage 3 liver cancer, there is still a need for ongoing research to improve outcomes for patients. Researchers are exploring new treatment options, including combination therapies that target multiple pathways involved in cancer growth and spread, immunotherapeutic approaches that harness the body’s immune system to fight cancer, and precision medicine that tailors treatment based on the individual’s genetic makeup.
Clinical trials are also underway to evaluate the safety and efficacy of these emerging therapies. These trials involve testing new drugs or drug combinations, as well as new approaches to surgery and radiation therapy, to determine their effectiveness in improving survival rates and quality of life for patients with stage 3 liver cancer.
In the coming years, advancements in biomarker research may also lead to new diagnostic tools that can detect liver cancer at an earlier stage, when treatment options are more effective. Additionally, the use of artificial intelligence and machine learning may help healthcare providers better predict patient outcomes and develop personalized treatment plans.
Looking ahead, the future of stage 3 liver cancer treatment and prognosis appears promising. While there is still much work to be done, ongoing research and clinical trials offer hope for advancing therapies that improve outcomes and quality of life for patients.
FAQ
What is the life expectancy for individuals with stage 3 liver cancer?
The life expectancy for individuals diagnosed with stage 3 liver cancer can vary depending on various factors. It is important to consult with a healthcare professional who can provide personalized information based on your specific case.
What factors can influence the life expectancy of individuals with stage 3 liver cancer?
Several factors can impact the life expectancy of individuals with stage 3 liver cancer. These may include the size and number of tumors, involvement of nearby lymph nodes, the extent of cancer spread, age, overall health, response to treatment, and the presence of underlying health conditions.
What are the treatment options for stage 3 liver cancer?
The treatment options for stage 3 liver cancer can include surgical interventions, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. The appropriate treatment plan will depend on several factors and should be discussed with a healthcare professional.
How can surgery be used to treat stage 3 liver cancer?
Surgery can be utilized for stage 3 liver cancer through procedures such as resection, liver transplantation, and ablation techniques. The specific approach will depend on individual circumstances, and it is best to consult with a surgeon who specializes in liver cancer treatment.
What is radiation therapy and how can it be used for stage 3 liver cancer?
Radiation therapy involves using high-energy beams to target and kill cancer cells. It can be used to treat stage 3 liver cancer by shrinking tumors or relieving symptoms. The specific radiation techniques and their effectiveness will be determined by a radiation oncologist.
How does chemotherapy play a role in the treatment of stage 3 liver cancer?
Chemotherapy uses drugs to destroy cancer cells or slow down their growth. It can be an option for stage 3 liver cancer, and the specific chemotherapy drugs, administration methods, and potential side effects will be determined by an oncologist.
What is targeted therapy and how is it used for stage 3 liver cancer?
Targeted therapy is a type of treatment that targets specific molecules or pathways involved in the growth of cancer cells. It can be used for stage 3 liver cancer, and the specific targeted therapy drugs, side effects, and ongoing research in this area can be discussed with an oncologist.
Can immunotherapy be utilized for the treatment of stage 3 liver cancer?
Immunotherapy aims to enhance the body’s immune system to fight against cancer cells. It can be used as a treatment option for stage 3 liver cancer, and the specific immunotherapeutic approaches, mechanisms of action, and potential benefits will be assessed by an oncologist.
What are the survival rates associated with stage 3 liver cancer?
Survival rates for stage 3 liver cancer can vary depending on individual cases. It is important to consult with a healthcare professional who can provide specific information based on the latest research and prognostic factors.
How can individuals cope with stage 3 liver cancer?
Coping with stage 3 liver cancer can be challenging, and it is important to have a strong support network in place. Strategies for coping may include seeking emotional support, joining support groups, accessing resources for practical assistance, and maintaining a positive mindset.
What role do palliative care and hospice services play in managing stage 3 liver cancer?
Palliative care focuses on improving the quality of life for individuals with serious illnesses, including stage 3 liver cancer. Hospice services provide comprehensive end-of-life care and support. These services can provide pain relief, symptom management, emotional support, and assistance for patients and their families.
What are the current research and future perspectives in the field of stage 3 liver cancer treatment and prognosis?
Ongoing research and clinical trials are continuously advancing the understanding and treatment of stage 3 liver cancer. There are promising developments in areas such as targeted therapies, immunotherapies, and multidisciplinary approaches. It is advisable to consult with a healthcare professional or participate in clinical trials to explore these emerging options.