Welcome to our comprehensive guide on the treatment options available for stage 3 cervical cancer. In this article, we will explore various approaches to managing this condition, focusing on their effectiveness and benefits. Understanding the treatment landscape is crucial for individuals and their loved ones facing stage 3 cervical cancer, as it empowers them to make informed decisions regarding their care.
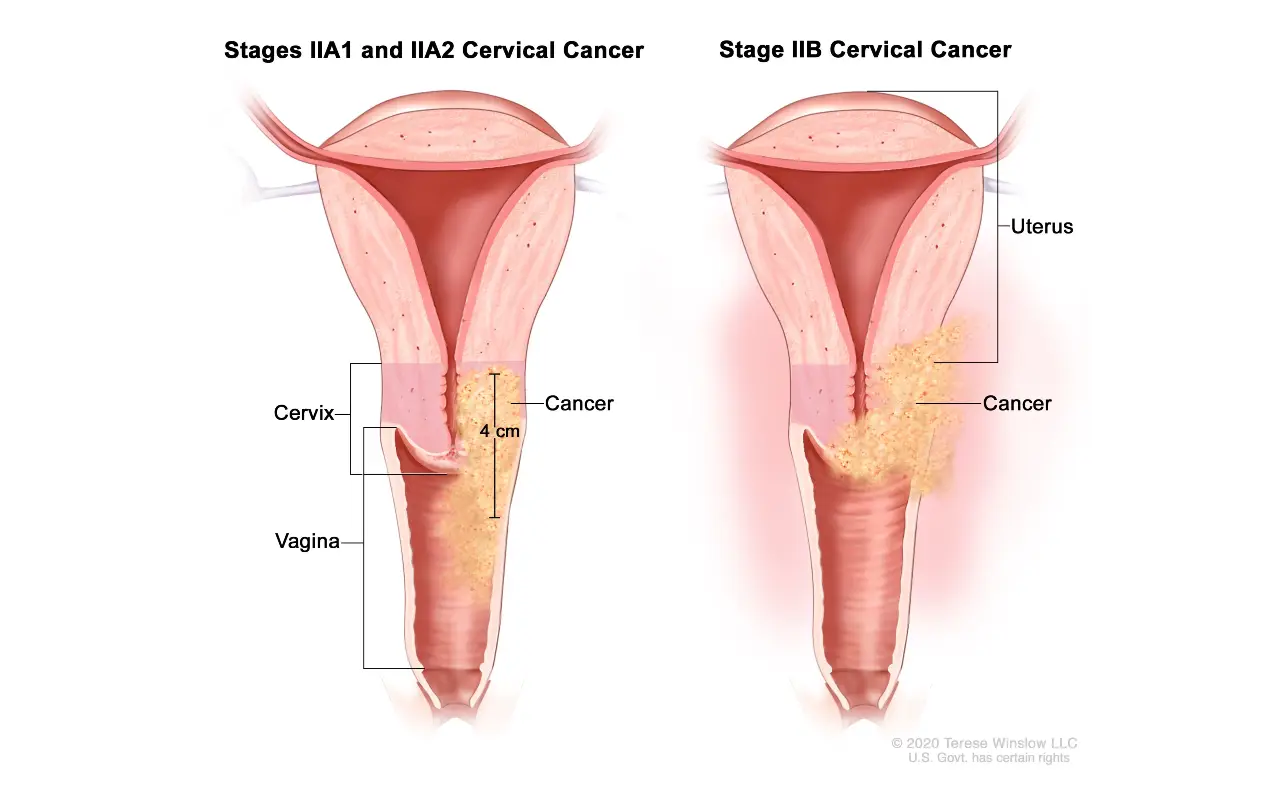
Stage 3 cervical cancer is an advanced form of the disease, where cancer cells have spread to nearby tissues and potentially to the lymph nodes. Treatment aims to eradicate or control the cancer, alleviate symptoms, and improve quality of life. It typically involves a combination of different modalities based on the individual’s specific circumstances and medical recommendations.
In the following sections, we will delve into each treatment option, examining its role in addressing stage 3 cervical cancer:
Surgery as a Treatment Option
Surgery plays a crucial role in the treatment of stage 3 cervical cancer. It offers a direct approach to removing cancerous cells and can be used as a standalone treatment or in combination with other therapies. Two primary surgical interventions for stage 3 cervical cancer are radical hysterectomy and lymph node dissection.
Radical Hysterectomy
A radical hysterectomy involves the removal of the cervix, uterus, upper vagina, and surrounding tissues where the cancer may have spread. This procedure is typically performed under general anesthesia and may require a hospital stay of several days. The goal of a radical hysterectomy is to eliminate the tumor and reduce the risk of cancer recurrence.
Lymph Node Dissection
To assess the spread of cancer, lymph node dissection, also known as lymphadenectomy, may be performed during a radical hysterectomy. This procedure involves the removal of pelvic and/or para-aortic lymph nodes for pathological examination. Lymph node dissection helps determine the stage of cancer and guides further treatment decisions.
It is important to note that surgery may not be suitable for all patients with stage 3 cervical cancer. Factors such as overall health, age, and the extent of cancer spread are taken into consideration when determining the most appropriate treatment approach. A comprehensive evaluation by a multidisciplinary team of healthcare professionals helps tailor the treatment plan to individual needs.
| Surgical Option | Description |
|---|---|
| Radical Hysterectomy | Removal of the cervix, uterus, upper vagina, and surrounding tissues |
| Lymph Node Dissection | Removal of pelvic and/or para-aortic lymph nodes for pathological examination |
Radiation Therapy for Stage 3 Cervical Cancer
Radiation therapy plays a crucial role in the treatment of stage 3 cervical cancer. It can be employed as a primary therapy or used alongside other treatment modalities to effectively target cancer cells and reduce tumor size. Radiation therapy utilizes high-energy beams or radioactive sources to destroy cancer cells and prevent their further growth.
Benefits of Radiation Therapy:
- Targets cancer cells in the cervix, uterus, and nearby lymph nodes
- Effective in reducing tumor size and controlling the spread of cancer
- Can be used as a curative treatment option in some cases
- Minimally invasive compared to surgery
- Preserves fertility in select patients
Potential Side Effects:
While radiation therapy is an effective treatment option, it may also have some side effects. These can vary depending on the type and duration of treatment, as well as individual patient factors. Potential side effects of radiation therapy for stage 3 cervical cancer include:
| Side Effects | Description |
|---|---|
| Fatigue | The feeling of physical and mental tiredness |
| Skin Changes | Redness, dryness, or darkening of the skin in the treatment area |
| Nausea and Vomiting | The feeling of sickness and involuntary emptying of the stomach |
| Bladder and Bowel Changes | Increased frequency, urgency, or discomfort during urination or bowel movements |
| Sexual Dysfunction | Changes in sexual desire or function |
| Fertility Issues | Possible impact on fertility, depending on treatment approach |
It is important to remember that not all patients will experience these side effects, and their severity can vary from person to person. Healthcare providers will closely monitor patients undergoing radiation therapy to manage and alleviate any potential side effects.
Chemotherapy and Its Role in Treating Stage 3 Cervical Cancer
In the treatment of stage 3 cervical cancer, chemotherapy plays a vital role in targeting cancer cells and reducing the risk of recurrence. Administered through various delivery methods, chemotherapy drugs are designed to destroy cancer cells while minimizing damage to healthy tissues.
Chemotherapy can be used as a primary treatment for stage 3 cervical cancer or as an adjuvant therapy after surgery or radiation. It can be delivered in different forms, such as intravenous infusion, oral medication, or directly into the affected area.
One of the primary chemotherapy regimens used for stage 3 cervical cancer is a combination of cisplatin and paclitaxel. These drugs work together to inhibit the growth and division of cancer cells, preventing them from spreading further.
While chemotherapy is effective in treating stage 3 cervical cancer, it can also present certain side effects, which may vary depending on the individual and the specific drugs used. Common side effects include fatigue, nausea, hair loss, and lowered blood cell counts. However, it is essential to note that side effects can be managed with supportive medications and interventions.
In some cases, concurrent chemoradiotherapy may be recommended, where chemotherapy is combined with radiation therapy to enhance treatment outcomes. This multidisciplinary approach aims to boost the effectiveness of both therapies, increasing the chances of successful cancer treatment.
Patients need to discuss chemotherapy treatment options, potential side effects, and supportive care measures with their healthcare team. Understanding the benefits and risks of chemotherapy can help individuals make informed decisions about their treatment plans.
Key Points:
- Chemotherapy is a vital treatment modality for stage 3 cervical cancer.
- It can be used as a primary therapy or in conjunction with surgery or radiation.
- A combination of cisplatin and paclitaxel is commonly used to target cancer cells.
- Side effects of chemotherapy can be managed with supportive care measures.
- Concurrent chemoradiotherapy may be recommended to enhance treatment outcomes.
Targeted Therapy for Stage 3 Cervical Cancer
In the treatment of stage 3 cervical cancer, targeted therapy has emerged as a promising approach. This innovative treatment option aims to selectively target cancer cells while minimizing damage to healthy cells, thereby enhancing the effectiveness of cancer treatment. Targeted therapies for stage 3 cervical cancer primarily involve the use of immune checkpoint inhibitors and angiogenesis inhibitors.
Immune Checkpoint Inhibitors
Immune checkpoint inhibitors are a type of targeted therapy that works by blocking proteins that can prevent the immune system from effectively attacking cancer cells. In stage 3 cervical cancer, immune checkpoint inhibitors such as pembrolizumab and nivolumab have shown promising results in clinical trials, with improved response rates and prolonged survival observed in some patients.
Angiogenesis Inhibitors
Angiogenesis inhibitors are targeted therapies that aim to prevent the formation of new blood vessels, which are crucial for the growth and spread of tumors. By inhibiting angiogenesis, these therapies can effectively reduce the blood supply to cancer cells, thereby restricting their ability to grow and metastasize. Bevacizumab is one such angiogenesis inhibitor that has been studied in the context of stage 3 cervical cancer, demonstrating potential benefits in combination with standard chemotherapy regimens.
| Targeted Therapy | Benefits | Potential Side Effects |
|---|---|---|
| Immune Checkpoint Inhibitors (e.g., pembrolizumab, nivolumab) | – Enhanced immune response against cancer cells – Improved response rates and survival in some patients |
– Fatigue – Rash – Immune-related adverse effects |
| Angiogenesis Inhibitors (e.g., bevacizumab) | – Reduced blood supply to tumors – Potential benefits in combination with chemotherapy |
– High blood pressure – Increased risk of bleeding – Gastrointestinal perforation |
It is important to note that targeted therapies for stage 3 cervical cancer are still under investigation, and their precise role in treatment is being defined through ongoing research and clinical trials. Additionally, like any cancer treatment, targeted therapies can have side effects that vary depending on the individual. Therefore, patients must have thorough discussions with their healthcare team to understand the potential benefits, risks, and suitability of targeted therapy as part of their overall treatment plan.
Emerging Therapies for Stage 3 Cervical Cancer
In recent years, there has been significant progress in the development of emerging therapies for stage 3 cervical cancer. Researchers and medical professionals are exploring innovative approaches, such as immunotherapy and gene therapy, to improve treatment outcomes and enhance the quality of life for patients.
Immunotherapy: Harnessing the Power of the Immune System
Immunotherapy has emerged as a promising treatment option for stage 3 cervical cancer. It works by stimulating the patient’s immune system to recognize and attack cancer cells more effectively. This approach has shown encouraging results in clinical trials, with some patients experiencing prolonged survival rates and improved response to treatment.
Gene Therapy: Targeting Cancer at the Molecular Level
Another exciting area of research is gene therapy, which involves introducing genetic material into cancer cells to inhibit their growth or induce cell death. By targeting specific genes or molecular pathways, gene therapy holds the potential to disrupt the mechanisms that allow cancer cells to survive and proliferate. While still in the early stages of development, initial studies have shown promising results in preclinical models.
As research continues to progress, it is important to note that emerging therapies are not yet widely available and may only be accessible through clinical trials or specialized centers. However, these advancements offer hope for future treatment options and underline the ongoing commitment to finding new approaches to combat stage 3 cervical cancer.
| Treatment | Potential Benefits | Current Status |
|---|---|---|
| Immunotherapy | Enhanced immune response, improved survival rates | Undergoing clinical trials, limited availability |
| Gene Therapy | Inhibition of cancer cell growth, potential for targeted treatment | Early stages of development, preclinical studies |
While emerging therapies hold great promise, it is important to acknowledge that further research and clinical trials are needed to determine their safety and long-term efficacy. Patients need to consult with their healthcare providers to access the most appropriate and up-to-date treatment options for stage 3 cervical cancer.
Clinical Trials and Experimental Treatments
In the quest for innovative and effective treatments for stage 3 cervical cancer, clinical trials play a vital role. These trials, conducted by researchers and healthcare professionals, aim to evaluate the safety and efficacy of experimental treatments. Through participation in clinical trials, patients have the opportunity to access cutting-edge therapies that may otherwise not be available.
Researchers design clinical trials to explore new treatment approaches, refine existing therapies, and uncover potential breakthroughs in cancer management. These trials adhere to strict protocols and guidelines to ensure patient safety and reliable data collection.
In the field of stage 3 cervical cancer, various clinical trials are underway, testing novel treatments and interventions. These trials often involve the use of targeted therapies, immunotherapy agents, and combination therapies to enhance treatment outcomes. By investigating these experimental treatments, researchers aim to advance the understanding of the disease and improve patient outcomes.
Participating in a clinical trial for stage 3 cervical cancer offers several potential benefits. It provides access to innovative treatments before they become widely available, and it allows patients to contribute to the development of improved therapies. Additionally, patients in clinical trials receive close medical supervision and comprehensive care from a multidisciplinary team.
To find clinical trials for stage 3 cervical cancer, patients can consult their healthcare providers or visit reputable online resources, such as the National Cancer Institute’s Clinical Trials Database. These resources provide information about ongoing trials, inclusion criteria, and contact details for trial coordinators.
Ongoing Clinical Trials for Stage 3 Cervical Cancer
| Study Title | Treatment Approach | Status |
|---|---|---|
| Phase III Trial of Chemotherapy plus Radiation Therapy with or without Bevacizumab in Patients with Locally Advanced Cervical Cancer | Chemotherapy, radiation therapy, bevacizumab (angiogenesis inhibitor) | Ongoing, recruiting participants |
| Phase II Study of Pembrolizumab (PD-1 Blockade) in Combination with Chemotherapy for Persistent, Recurrent, or Metastatic Cervical Cancer | Pembrolizumab (immune checkpoint inhibitor), chemotherapy | Ongoing, recruiting participants |
| Phase I Study of Gene Therapy for Locally Advanced Cervical Cancer | Gene therapy | Ongoing, recruiting participants |
Note: This table provides a snapshot of ongoing clinical trials for stage 3 cervical cancer and does not represent an exhaustive list. The status of trials may change, and participation criteria may vary. It is advisable to consult healthcare professionals or research coordinators for the most up-to-date information.
Palliative Care and Supportive Treatments
Palliative care and supportive treatments play a critical role in improving the quality of life for individuals with stage 3 cervical cancer. These approaches focus on providing comprehensive care that addresses both physical and emotional needs, aiming to enhance comfort and overall well-being.
Pain Management
Effective pain management is a crucial aspect of palliative care for individuals with stage 3 cervical cancer. This involves a multidisciplinary approach that may include medications, such as opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and antidepressants, as well as interventions like nerve blocks and physical therapy. Specialized techniques like acupuncture and massage therapy can also offer relief and promote relaxation.
Emotional Support
The emotional impact of a stage 3 cervical cancer diagnosis can be overwhelming. Palliative care teams are equipped to provide emotional and psychological support to patients and their families, helping them navigate through the challenges and uncertainties they may face. Supportive therapies such as counseling, support groups, and mindfulness techniques can offer comfort and aid in coping with anxiety, depression, and stress.
Social Support
Social support is vital for individuals with stage 3 cervical cancer to feel connected, acknowledged, and understood. Palliative care teams can help patients and their families access community resources, support groups, and peer networks where they can find solace, share experiences, and gain valuable insights. Encouraging participation in such supportive communities can provide a sense of belonging and foster a positive outlook.
Advance Care Planning
As part of the palliative care approach, individuals with stage 3 cervical cancer are encouraged to engage in advance care planning. This involves open and honest discussions about treatment options, personal values, and goals of care. By proactively addressing end-of-life preferences and documenting healthcare decisions, patients can have peace of mind knowing that their wishes will be respected.
| Palliative Care and Supportive Treatments | Benefits |
|---|---|
| Pain management | Reduced discomfort and improved quality of life |
| Emotional support | Enhanced psychological well-being and better coping mechanisms |
| Social support | Increased sense of belonging and a support system for patients and their families |
| Advance care planning | Ensuring personal values and healthcare decisions are honored |
Integrative Medicine and Complementary Therapies
Integrative medicine and complementary therapies play a significant role in supporting individuals during their treatment journey for stage 3 cervical cancer. These approaches focus on enhancing overall well-being and promoting holistic healing, with a particular emphasis on the mind-body connection. By combining conventional medical treatments with evidence-based complementary practices, patients can experience improved quality of life and reduced side effects.
The Role of Integrative Medicine
Integrative medicine encompasses an approach that combines conventional medical treatments with complementary therapies to address the physical, emotional, and spiritual needs of patients. By incorporating practices such as acupuncture, massage therapy, and herbal supplements, integrative medicine aims to enhance the body’s natural healing mechanisms and support the effectiveness of conventional treatments.
Research has shown that integrative medicine can provide numerous benefits for individuals with stage 3 cervical cancer. For example, acupuncture has been found to alleviate chemotherapy-induced nausea and vomiting, while massage therapy can help reduce stress, pain, and anxiety. Additionally, mind-body techniques like yoga and meditation have been shown to improve overall well-being and quality of life.
The Role of Complementary Therapies
Complementary therapies, also known as alternative therapies, work alongside traditional medical treatments to provide additional support and symptom management. These therapies encompass various modalities, including herbal medicine, aromatherapy, and nutritional supplements.
Specific complementary therapies, such as acupuncture and yoga, have gained recognition for their potential benefits in managing side effects and improving overall outcomes for individuals with stage 3 cervical cancer. Acupuncture can help alleviate pain, reduce fatigue, and improve sleep quality. Yoga, on the other hand, promotes flexibility, reduces stress, and enhances emotional well-being.
Collaborative Care and Consultation
It is essential for individuals considering integrative medicine and complementary therapies to work closely with their healthcare team. Open communication and collaboration between healthcare providers and complementary therapy practitioners ensure that all aspects of the patient’s care are coordinated and aligned to optimize treatment outcomes.
Patients should consult with their oncologists and other healthcare professionals before incorporating any complementary therapies into their treatment plans. This collaboration helps to ensure the safe and effective integration of complementary therapies into the overall care strategy.
The Table below provides an overview of common integrative medicine and complementary therapies used in the treatment of stage 3 cervical cancer:
| Integrative Medicine | Complementary Therapies |
|---|---|
| Acupuncture | Herbal medicine |
| Mind-body techniques (yoga, meditation) | Aromatherapy |
| Massage therapy | Nutritional supplements |
Psychological Support and Counseling
Psychological support and counseling play a crucial role in the comprehensive care of individuals with stage 3 cervical cancer. Coping with a cancer diagnosis and undergoing treatment can lead to increased emotional distress and mental health challenges. Access to professional psychological support and counseling services can help individuals navigate these difficult emotions, manage stress, and promote overall well-being.
Psychological support services provide a safe and confidential space for individuals to express their fears, anxieties, and concerns about their condition. These services are delivered by qualified mental health professionals who specialize in providing emotional support to cancer patients. The goal is to help patients develop coping strategies and tools to navigate the emotional impact of their diagnosis and treatment.
Counseling sessions can address a range of psychological and emotional issues, including anxiety, depression, grief, body image concerns, and relationship difficulties. Additionally, counseling can help individuals develop effective communication and coping skills, build resilience, and foster a positive mindset during their cancer journey.
The Benefits of Psychological Support and Counseling
The benefits of psychological support and counseling for individuals with stage 3 cervical cancer are numerous. Here are some key benefits:
- Helps manage anxiety and depression associated with a cancer diagnosis
- Provides a supportive environment to express fears, concerns, and emotions
- Assists in developing effective coping strategies for managing stress
- Improves overall emotional well-being and quality of life
- Enhances communication skills with healthcare providers, family, and friends
- Promotes a positive mindset and resilience
It is important to note that psychological support and counseling should be tailored to the individual’s specific needs and preferences. This may include individual counseling sessions, group therapy, or a combination of both. The frequency and duration of counseling sessions may vary depending on the individual’s requirements and treatment plan.
By addressing the emotional aspects of living with stage 3 cervical cancer, psychological support, and counseling can significantly improve the overall well-being and quality of life for individuals facing this challenging disease.
Overview of Psychological Support and Counseling Services
| Services | Description |
|---|---|
| Individual Counseling | One-on-one sessions with a qualified mental health professional to address specific emotional needs and concerns. |
| Group Therapy | Participation in group sessions with other individuals facing similar challenges, providing a supportive and understanding environment. |
| Family Counseling | Sessions that involve family members to improve communication, address relationship issues, and strengthen support networks. |
| Support Groups | Facilitated gatherings where individuals can share experiences, gain practical advice, and find comfort in a community of peers. |
| Cognitive-Behavioral Therapy | A type of therapy that focuses on identifying and changing negative thought patterns and behaviors to promote emotional well-being. |
Support Groups and Peer Networks
Support groups and peer networks play a crucial role in the journey of individuals affected by stage 3 cervical cancer. These communities provide a sense of belonging, understanding, and empathy, helping patients, survivors, and their loved ones navigate the challenges associated with the disease.
When facing a diagnosis of stage 3 cervical cancer, it is common to feel overwhelmed and isolated. Joining a support group can help alleviate these feelings by connecting individuals going through similar experiences. In these groups, participants can share their stories and emotions, finding solace in the support and understanding of others who truly comprehend the physical and emotional impact of the condition.
Support groups offer a safe space for individuals to express their fears, anxieties, and triumphs while receiving encouragement and guidance. Participants often develop strong bonds and lifelong friendships through these shared experiences. Members uplift each other, providing a network of emotional support during every stage of the cancer journey.
Additionally, support groups provide practical advice and valuable insights. Members can exchange information about treatment options, coping strategies, and helpful resources, allowing individuals to make more informed decisions about their care and well-being. Peer networks offer a diverse range of perspectives and experiences, enabling participants to benefit from a wealth of knowledge.
Benefits of Support Groups and Peer Networks:
- Emotional Support: Individuals can share their thoughts and feelings, receive encouragement, and gain a sense of belonging from others who understand their challenges.
- Practical Advice and Information: Support groups offer a platform for members to exchange knowledge about treatment options, managing side effects, and accessing supportive resources.
- Shared Experiences: Participants can connect with others facing similar journeys, fostering a sense of camaraderie and understanding that is crucial for overall well-being.
- Promoting Mental Health: Peer networks provide opportunities for individuals to discuss the emotional impact of the disease and learn coping strategies to navigate the psychological challenges.
- Building Resilience and Empowerment: Support from peers can help individuals build resilience, regain a sense of control, and feel empowered throughout their cancer experience.
In conclusion, support groups and peer networks form an invaluable part of the comprehensive care and support system for those affected by stage 3 cervical cancer. These communities not only provide emotional support but also offer practical advice, shared experiences, and a sense of empowerment. By fostering a strong network of support, individuals facing stage 3 cervical cancer can find comfort, knowledge, and the strength to navigate their journey with confidence.
Lifestyle Factors and Recommendations
Adopting a healthy lifestyle can play a crucial role in improving treatment outcomes for individuals with stage 3 cervical cancer. Making positive changes in diet, exercise, and stress management can have a significant impact on overall well-being and aid in the healing process.
Dietary Recommendations
A well-balanced diet rich in nutrients can help support the immune system and contribute to better treatment response. Here are some dietary recommendations for individuals with stage 3 cervical cancer:
- Focus on consuming a variety of fruits and vegetables that are high in antioxidants, vitamins, and minerals.
- Incorporate whole grains, lean proteins, and healthy fats into your meals.
- Avoid processed foods, sugary snacks, and excessive intake of red and processed meats.
- Stay hydrated by drinking an adequate amount of water throughout the day.
Exercise Tips
Maintaining an active lifestyle can offer numerous benefits during cancer treatment, including improved mood, increased energy levels, and enhanced overall physical well-being. It is essential to consult with your healthcare team before starting any exercise regimen. Here are some exercise tips:
- Engage in regular moderate-intensity exercises such as brisk walking, swimming, or cycling.
- Consider incorporating strength training exercises to improve muscle strength and flexibility.
- Listen to your body and adjust the intensity and duration of exercise based on your energy levels and physical capabilities.
Stress Management Strategies
Chronic stress can hurt both physical and mental health. Incorporating effective stress management strategies can help reduce anxiety, improve sleep quality, and enhance overall well-being. Here are some recommendations:
- Practice relaxation techniques such as deep breathing exercises, meditation, or yoga.
- Find activities that bring you joy and help you relax, such as engaging in hobbies, listening to music, or spending time in nature.
- Seek support from friends, family, or professional counselors to help manage emotional stressors.
By implementing these lifestyle factors and recommendations, individuals with stage 3 cervical cancer can strive for a healthier and more balanced life, complementing their medical treatment and improving their overall well-being.
| Lifestyle Factors | Recommendations |
|---|---|
| Diet | Include a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats in your diet. Avoid processed foods, sugary snacks, and excessive intake of red and processed meats. |
| Exercise | Engage in regular moderate-intensity exercises such as brisk walking, swimming, or cycling. Consider incorporating strength training exercises to improve muscle strength and flexibility. |
| Stress Management | Practice relaxation techniques such as deep breathing exercises, meditation, or yoga. Find activities that bring you joy and help you relax. Seek support from friends, family, or professional counselors. |
Follow-Up Care and Survivorship
After completing treatment for stage 3 cervical cancer, individuals must prioritize long-term follow-up care and survivorship plans. These crucial aspects play a significant role in monitoring potential recurrent or new cancer developments, managing late effects, and ensuring overall well-being.
Regular surveillance is essential for detecting any signs of cancer recurrence promptly. Follow-up care typically involves scheduled appointments with healthcare professionals, including gynecologic oncologists, oncology nurses, and radiation oncologists. These visits may include physical examinations, imaging tests such as CT scans or MRIs, and bloodwork to assess tumor markers or other relevant indicators.
Aside from monitoring for cancer recurrence, survivorship care also focuses on managing potential late effects of treatment. Depending on the specific treatments received, individuals may experience side effects such as lymphedema, early menopause, sexual dysfunction, or emotional challenges. Healthcare providers will offer guidance and support to address these concerns, ensuring optimal survivorship and quality of life.
In addition to medical care, survivorship plans also emphasize healthy lifestyle choices. This may include recommendations for a balanced diet, regular exercise, and stress reduction strategies. Adopting these practices can help improve overall well-being and reduce the risk of cancer recurrence or other health complications.
FAQ
What are the treatment options for stage 3 cervical cancer?
The treatment options for stage 3 cervical cancer may include surgery, radiation therapy, chemotherapy, targeted therapy, and emerging therapies. The choice of treatment depends on various factors, such as the extent of the cancer, overall health, and personal preferences.
What is the role of surgery in treating stage 3 cervical cancer?
Surgery can be a treatment option for stage 3 cervical cancer and may involve procedures like radical hysterectomy and lymph node dissection. These surgeries aim to remove the cancerous cells and nearby lymph nodes to prevent the spread of the disease.
How is radiation therapy used in the management of stage 3 cervical cancer?
Radiation therapy can be used as a primary treatment or in combination with other modalities for stage 3 cervical cancer. It involves the use of high-energy rays to kill cancer cells or shrink tumors. Radiation therapy can be delivered externally or internally through brachytherapy.
What is the role of chemotherapy in treating stage 3 cervical cancer?
Chemotherapy drugs can be administered to individuals with stage 3 cervical cancer either alone or in conjunction with other treatments like surgery or radiation therapy. Chemotherapy aims to destroy cancer cells or impede their growth, often using a combination of drugs.
What is targeted therapy, and how does it relate to stage 3 cervical cancer?
Targeted therapy is a treatment approach that focuses on specific molecules or pathways involved in the growth of cancer cells. In the case of stage 3 cervical cancer, targeted therapy options like immune checkpoint inhibitors and angiogenesis inhibitors can be used to disrupt the growth and spread of cancer cells.
Are there any emerging therapies being studied for stage 3 cervical cancer?
Yes, researchers are exploring new treatment approaches, including immunotherapy and gene therapy, for the management of stage 3 cervical cancer. These emerging therapies hold promise in enhancing treatment outcomes and expanding the treatment options available.
What role do clinical trials play in the treatment of stage 3 cervical cancer?
Clinical trials are vital in advancing the understanding and treatment of stage 3 cervical cancer. They provide opportunities for individuals to access experimental treatments and contribute to the development of future therapies. Participation in clinical trials is voluntary and usually guided by eligibility criteria.
How do palliative care and supportive treatments benefit individuals with stage 3 cervical cancer?
Palliative care and supportive treatments play a crucial role in improving the quality of life for individuals with stage 3 cervical cancer. These services focus on addressing pain, managing symptoms, and providing emotional and psychological support throughout the treatment journey.
What is integrative medicine, and how does it complement conventional treatments for stage 3 cervical cancer?
Integrative medicine integrates complementary therapies, such as acupuncture and yoga, with conventional medical treatments. It aims to enhance overall well-being and may help manage treatment-related side effects, reduce stress, and improve the overall treatment experience for individuals with stage 3 cervical cancer.
Why is psychological support and counseling important for individuals with stage 3 cervical cancer?
Psychological support and counseling services are essential for individuals with stage 3 cervical cancer as they provide a safe space for emotional expression and help individuals cope with the challenges associated with the disease. These services can significantly impact mental well-being and overall treatment outcomes.
How can support groups and peer networks assist individuals affected by stage 3 cervical cancer?
Support groups and peer networks offer a sense of community, provide shared experiences, and offer practical advice for individuals affected by stage 3 cervical cancer. They can act as a valuable source of support, guidance, and inspiration throughout the treatment journey.
What lifestyle factors can enhance treatment outcomes for individuals with stage 3 cervical cancer?
Adopting a healthy lifestyle can have a positive impact on treatment outcomes for individuals with stage 3 cervical cancer. This may include following a balanced diet, engaging in regular exercise, managing stress, and avoiding harmful habits like smoking.
Why is follow-up care and survivorship important for individuals who have completed treatment for stage 3 cervical cancer?
Follow-up care and survivorship plans are crucial for individuals who have completed treatment for stage 3 cervical cancer. They involve regular check-ups, surveillance for potential recurrence or late effects, and ongoing support to ensure the long-term well-being and overall health of the patient.