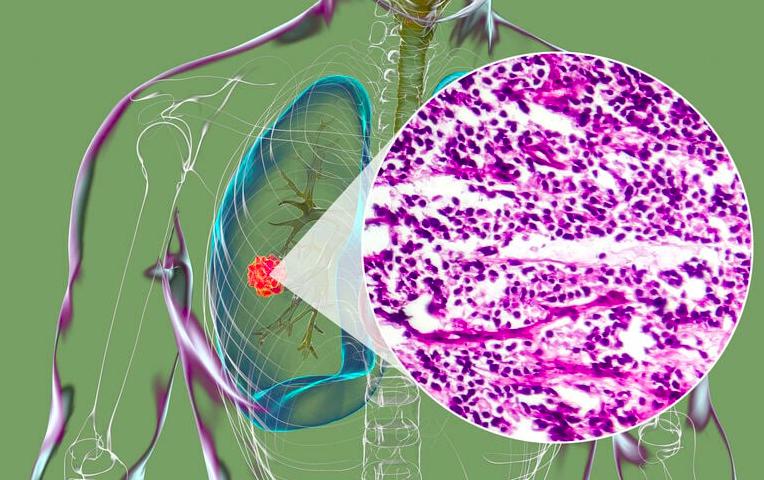
Small cell lung cancer (SCLC) is one of the most aggressive forms of lung cancer, accounting for about 10–15% of all lung cancer cases. Despite its rapid growth and tendency to spread early, advances in small cell lung cancer treatment have improved patient outcomes and quality of life. Understanding the disease, recognizing symptoms, and knowing the available treatment options are essential steps toward better management.
Patients diagnosed with SCLC often face overwhelming questions about survival, therapy choices, and lifestyle adjustments. This comprehensive guide explores everything from the causes and symptoms to the latest innovations in small cell lung cancer treatment, giving patients and caregivers the knowledge they need to make informed decisions.
Definition and Overview
Small cell lung cancer is a high-grade neuroendocrine tumor that develops in the lungs. Unlike non-small cell lung cancer, SCLC grows and spreads quickly, often reaching the lymph nodes and distant organs before diagnosis. Because of its aggressive nature, early detection is rare, and immediate treatment is crucial.
Types
There are two main stages of small cell lung cancer:
- Limited-stage SCLC: Cancer is confined to one side of the chest and can typically be targeted with localized treatment.
- Extensive-stage SCLC: Cancer has spread to other parts of the chest or distant organs, requiring systemic therapy.
Causes and Risk Factors
The primary cause of small cell lung cancer is tobacco smoking, responsible for the majority of cases. Other risk factors include:
- Exposure to secondhand smoke
- Radon gas exposure
- Occupational hazards such as asbestos
- Family history of lung cancer
- Weakened immune system
Symptoms and Early Warning Signs
SCLC symptoms often appear only after the cancer has advanced. Common signs include:
- Persistent cough
- Chest pain
- Shortness of breath
- Wheezing
- Fatigue
- Unexplained weight loss
- Swelling in the face or neck due to tumor pressure
Because of its rapid progression, recognizing these symptoms and seeking medical attention promptly is critical.
Diagnosis
Diagnosis of small cell lung cancer typically involves:
- Imaging tests: Chest X-ray, CT scan, and PET scan to detect tumors.
- Biopsy: Obtaining tissue samples to confirm cancer type.
- Bronchoscopy: Direct examination of the lungs.
- Blood tests: To assess overall health and detect markers.
- Staging tests: MRI or bone scans to check for metastasis.
Treatment Options
Treatment for small cell lung cancer depends on the stage and overall health of the patient. Common approaches include:
- Chemotherapy: The primary treatment, often using drugs like cisplatin or etoposide.
- Radiation therapy: Targeted to shrink tumors and relieve symptoms.
- Immunotherapy: Newer treatments such as immune checkpoint inhibitors that boost the body’s defenses.
- Surgery: Rarely used, typically only in very early stages.
- Palliative care: Focused on symptom relief and improving quality of life.
Prevention and Lifestyle Recommendations
While not all cases of SCLC can be prevented, risk reduction strategies include:
- Quitting smoking and avoiding tobacco in all forms
- Testing for radon exposure at home
- Using protective equipment in high-risk occupations
- Maintaining a healthy diet and regular exercise to strengthen immunity
- Regular health check-ups for high-risk individuals
Prognosis and Survival Rates
Small cell lung cancer has a poorer prognosis compared to non-small cell lung cancer due to its aggressive nature. The five-year survival rate is approximately:
- 20–25% for limited-stage SCLC
- Less than 5% for extensive-stage SCLC
Early detection and prompt small cell lung cancer treatment can improve survival and quality of life.
Latest Research and Innovations
Recent research has focused on:
- Targeted therapies: Precision medicine designed for specific genetic mutations.
- Immunotherapy advancements: Drugs like atezolizumab and durvalumab are showing promise.
- Combination therapies: Integrating chemotherapy, radiation, and immunotherapy for better outcomes.
- Clinical trials: Ongoing studies exploring new drugs and novel treatment combinations.
Coping and Support for Patients
A diagnosis of SCLC can be emotionally and physically challenging. Coping strategies include:
- Joining cancer support groups
- Seeking counseling or therapy
- Engaging in relaxation techniques like meditation and yoga
- Maintaining open communication with healthcare providers and family
- Accessing palliative care and nutritional support
Conclusion
Small cell lung cancer remains a difficult disease to treat due to its aggressive progression and early spread. However, advances in small cell lung cancer treatment—including chemotherapy, radiation, immunotherapy, and ongoing clinical trials—offer hope for patients. Awareness of symptoms, early diagnosis, and lifestyle changes are essential in improving survival rates and quality of life.
FAQ
1. What is the main treatment for small cell lung cancer?
Chemotherapy is the primary treatment, often combined with radiation therapy and immunotherapy.
2. Can small cell lung cancer be cured?
In rare cases, if detected early in the limited stage, small cell lung cancer may be curable with aggressive treatment. However, most cases are managed rather than cured.
3. How fast does small cell lung cancer spread?
SCLC spreads rapidly, often within weeks to months, which is why early diagnosis and immediate treatment are critical.
4. Is surgery an option for small cell lung cancer treatment?
Surgery is rarely used, except in very early stages before the cancer has spread.
5. What lifestyle changes help after treatment?
Quitting smoking, eating a nutrient-rich diet, exercising regularly, and attending follow-up appointments all help improve recovery and overall well-being.