Pancreatic cancer is one of the most aggressive and difficult-to-treat cancers, raising a critical question for many patients and their families: can pancreatic cancer be cured? While medical advancements have improved survival rates and treatment strategies, the journey toward a potential cure remains challenging. Understanding the nature of this disease, its risk factors, and available treatments can help patients make informed decisions.
In this article, we will explore the definition of pancreatic cancer, its symptoms, diagnosis, treatment options, and prevention strategies. We will also discuss prognosis, survival rates, and the latest research aimed at finding new therapies. If you are searching for clear, professional, and SEO-friendly information on whether pancreatic cancer can be cured, this guide provides a comprehensive overview.
Definition and Overview
Pancreatic cancer begins in the tissues of the pancreas, an organ located behind the stomach that plays a vital role in digestion and blood sugar regulation. This cancer often goes undetected in its early stages, making it particularly dangerous. The primary concern for many patients is whether pancreatic cancer can be cured, which largely depends on the stage at diagnosis and available treatments.
Types
There are two main types of pancreatic cancer:
- Exocrine tumors: The most common type, usually adenocarcinomas, starting in the ducts of the pancreas.
- Endocrine tumors (neuroendocrine tumors): Less common and often slower-growing, arising from hormone-producing cells.
Causes and Risk Factors
The exact cause of pancreatic cancer is not fully understood, but several risk factors increase the likelihood of developing it:
- Genetic mutations
- Family history of pancreatic cancer
- Smoking and heavy alcohol use
- Obesity and poor diet
- Chronic pancreatitis
- Advanced age
Symptoms and Early Warning Signs
Pancreatic cancer often shows few or no symptoms until it has progressed. Some early warning signs may include:
- Persistent abdominal or back pain
- Unexplained weight loss
- Loss of appetite
- Yellowing of the skin and eyes (jaundice)
- Nausea or vomiting
- Fatigue
Diagnosis
To determine whether pancreatic cancer can be treated or potentially cured, doctors rely on several diagnostic methods:
- Imaging tests such as CT scans, MRI, or ultrasound
- Endoscopic ultrasound (EUS) for detailed imaging
- Blood tests for tumor markers like CA 19-9
- Biopsy to confirm cancer cells
Treatment Options
The treatment of pancreatic cancer depends on the stage and type of the disease:
- Surgery: The only potential cure, especially if the tumor is detected early and can be removed completely.
- Chemotherapy and radiation therapy: Used to shrink tumors, slow progression, and relieve symptoms.
- Targeted therapy and immunotherapy: Emerging treatments designed to attack cancer cells more precisely.
- Palliative care: Focuses on improving quality of life when a cure is not possible.
Prevention and Lifestyle Recommendations
While not all cases are preventable, lifestyle changes can lower the risk:
- Avoid smoking and limit alcohol intake
- Maintain a healthy weight
- Eat a diet rich in fruits, vegetables, and whole grains
- Stay physically active
- Manage underlying conditions like diabetes and chronic pancreatitis
Prognosis and Survival Rates
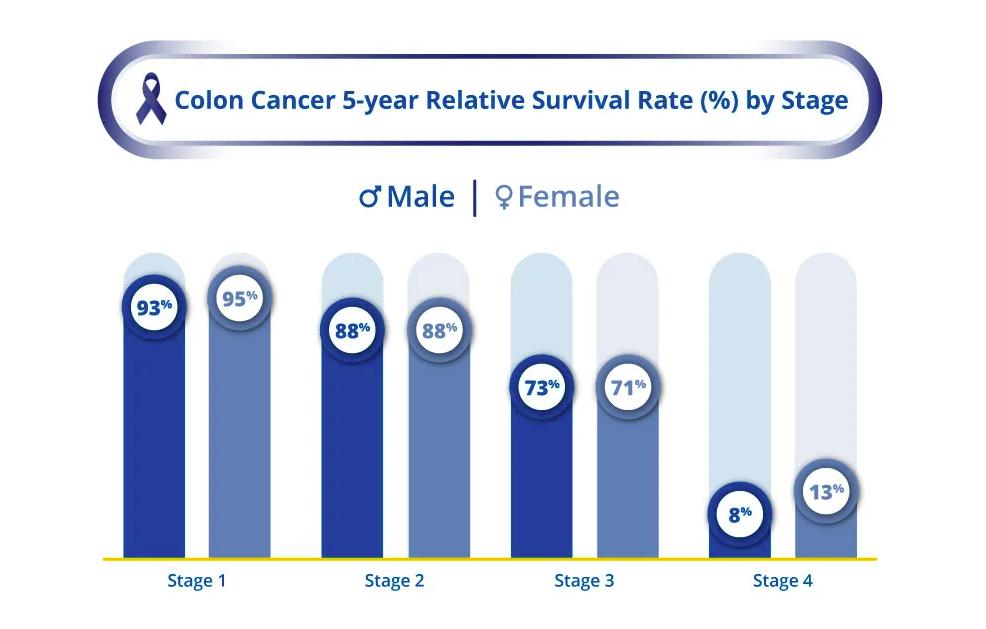
The prognosis for pancreatic cancer varies significantly. Unfortunately, survival rates remain low compared to other cancers due to late detection. The five-year survival rate is around 12%, but it can be higher for patients diagnosed at an early stage who undergo successful surgery. While a complete cure is rare, some patients achieve long-term remission with proper treatment.
Latest Research and Innovations
Ongoing research is exploring new ways to answer the question: can pancreatic cancer be cured? Advances include immunotherapy trials, personalized medicine based on genetic profiling, and targeted drugs that block cancer growth. Early detection methods using biomarkers and improved imaging are also showing promise.
Coping and Support for Patients
A pancreatic cancer diagnosis can be emotionally overwhelming. Patients and families should seek support through:
- Counseling and mental health care
- Patient support groups and online communities
- Nutritional guidance
- Palliative and hospice care when needed
Emotional and psychological support plays an essential role in improving the overall quality of life during treatment.
Conclusion
So, can pancreatic cancer be cured? While a complete cure remains rare, early detection combined with surgery and advanced treatments offers the best chance for long-term survival. Continued research and medical innovation bring hope for more effective therapies in the future. Patients are encouraged to work closely with healthcare providers, adopt healthy lifestyle habits, and seek emotional support throughout their journey.
FAQ
1. Can pancreatic cancer be cured completely?
A cure is possible in rare cases, usually when the cancer is detected early and surgically removed.
2. What is the life expectancy for pancreatic cancer patients?
Life expectancy varies depending on the stage, treatment response, and overall health, with early-stage patients having better outcomes.
3. What are the first signs of pancreatic cancer?
Common early signs include abdominal pain, jaundice, unexplained weight loss, and digestive issues.
4. Is surgery always an option for pancreatic cancer?
No, surgery is only possible if the tumor has not spread extensively and can be safely removed.
5. How can pancreatic cancer risk be reduced?
Adopting a healthy lifestyle, avoiding smoking, limiting alcohol, and managing chronic health conditions can lower the risk.