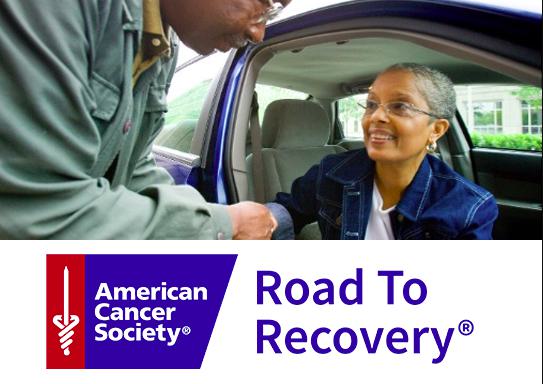
Cancer treatment is a difficult journey, and one of the most overlooked challenges patients face is transportation to and from medical appointments. Many patients struggle with reliable transportation, especially when multiple visits for chemotherapy, radiation, or follow-ups are required. The American Cancer Society Road to Recovery program was created to address this very issue, ensuring patients can access life-saving care without the barrier of transportation.
This initiative not only reduces stress for patients and families but also highlights the importance of community-driven support in the fight against cancer. By connecting volunteer drivers with patients in need, the program strengthens the healthcare system and provides a lifeline of hope for those battling cancer.
Definition and Overview
The American Cancer Society Road to Recovery is a volunteer-based program that offers free rides to cancer patients who need transportation to their treatment centers. It is designed for patients who do not have a ride, cannot drive themselves, or cannot afford transportation. By pairing patients with trained volunteer drivers, the program removes one of the most common non-medical barriers to cancer care.
Types
Although it is one unified program, the services under the Road to Recovery initiative can be categorized into:
- Volunteer Driver Program – Community members volunteer to drive patients to and from treatments.
- Patient Matching Services – The program coordinates scheduling to match patients with available drivers.
- Collaborative Partnerships – In some regions, the American Cancer Society partners with local transportation services or ride-share platforms to extend support.
Causes and Risk Factors
The need for Road to Recovery arises not from medical causes but from social and economic factors. Many cancer patients face:
- Lack of personal transportation
- Inability to drive due to illness or treatment side effects
- Limited financial resources for taxis or ride services
- Absence of family or friends to provide reliable rides
These barriers can delay or interrupt treatment, impacting recovery outcomes.
Symptoms and Early Warning Signs
While the Road to Recovery program itself is not a medical condition, it is closely tied to cancer care. Patients who need it often experience:
- Fatigue or weakness due to treatment
- Physical inability to drive safely
- Financial stress from ongoing care expenses
Recognizing these challenges early can help patients seek assistance before missing important appointments.
Diagnosis
The program identifies eligible participants through:
- Referrals from healthcare providers
- Patient self-enrollment via the American Cancer Society website or helpline
- Community outreach and local cancer support networks
Eligibility typically depends on the patient’s inability to secure safe transportation independently.
Treatment Options
While Road to Recovery is not a medical treatment, it plays a critical role in supporting treatment compliance. By providing dependable rides, it ensures patients can attend:
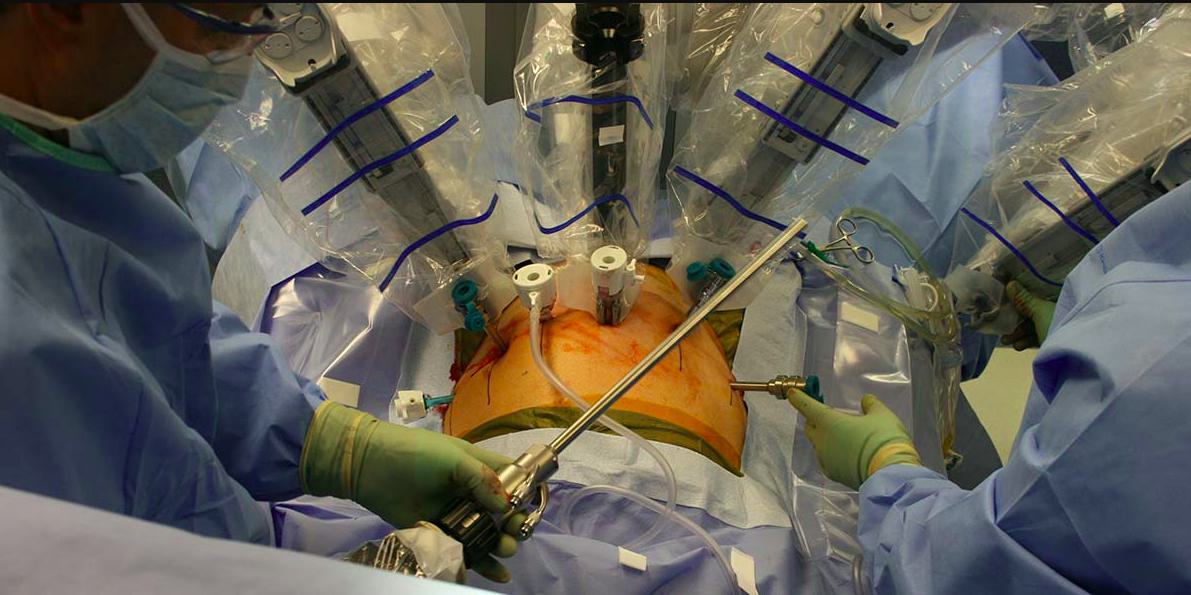
- Chemotherapy sessions
- Radiation therapy
- Follow-up appointments
- Counseling or support group meetings
Prevention and Lifestyle Recommendations
Prevention in this context means reducing barriers that prevent patients from accessing care. Patients and families are encouraged to:
- Plan transportation in advance of treatment cycles
- Explore volunteer opportunities to strengthen community support
- Maintain open communication with healthcare providers about logistical challenges
Prognosis and Survival Rates
Timely and consistent treatment improves survival rates and quality of life for cancer patients. Programs like American Cancer Society Road to Recovery indirectly boost prognosis by ensuring that patients do not miss critical treatments. Reliable transportation can make a measurable difference in overall health outcomes.
Latest Research and Innovations
The American Cancer Society continuously evaluates the impact of Road to Recovery. Recent innovations include:
- Use of digital platforms to match drivers and patients more efficiently
- Expansion of partnerships with ride-share companies to increase availability
- Data-driven approaches to identify communities with the greatest transportation needs
Coping and Support for Patients
Transportation assistance is more than just a ride; it provides emotional relief, reduces stress, and fosters a sense of community. Patients often find comfort knowing that volunteers and organizations care about their journey. Additionally, caregivers can feel less burdened, allowing them to focus more on emotional support.
Conclusion
The American Cancer Society Road to Recovery is a vital program that addresses one of the hidden struggles of cancer treatment—transportation. By ensuring that patients have reliable rides to their medical appointments, the program improves treatment adherence, reduces stress, and enhances survival outcomes. It stands as a testament to the power of community-driven support in the fight against cancer.
FAQ
1. What is the American Cancer Society Road to Recovery program?
It is a volunteer-driven initiative that provides free transportation for cancer patients to and from treatment centers.
2. Who is eligible for the Road to Recovery program?
Any cancer patient who cannot drive themselves or lacks reliable transportation may be eligible.
3. How do patients request a ride?
Patients can call the American Cancer Society helpline or apply online to schedule rides.
4. Is the service available everywhere in the U.S.?
Availability may vary by region depending on the number of volunteer drivers.
5. Can I volunteer as a driver?
Yes, community members can apply to become volunteer drivers through the American Cancer Society website.