Prostate cancer is one of the most common cancers affecting men worldwide. When diagnosed at stage 3, the disease has advanced beyond the prostate gland and may have spread to nearby tissues, making early recognition of symptoms and proper treatment essential. Understanding stage 3 prostate cancer symptoms is critical for detecting the disease early and improving treatment outcomes.
In this article, we’ll explore the key symptoms, causes, and treatment options for stage 3 prostate cancer, as well as practical advice on prevention and coping strategies. Whether you’re a patient, caregiver, or simply seeking information, this guide provides a comprehensive overview of everything you need to know about this condition.
Definition and Overview
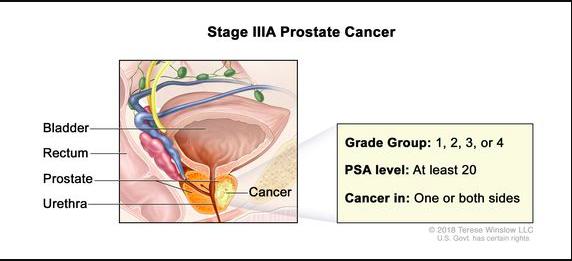
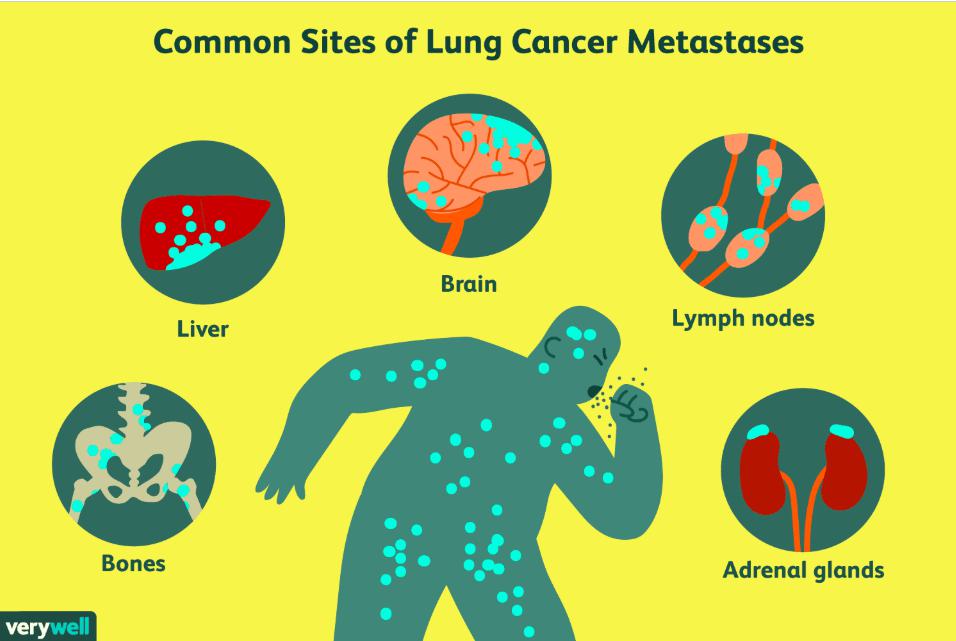
Stage 3 prostate cancer refers to a phase where the cancer has spread outside the prostate capsule but has not reached distant organs such as the lungs or bones. This stage is often divided into Stage 3A, 3B, and 3C, depending on the extent of tumor growth and the aggressiveness of cancer cells.
At this point, cancer may invade nearby structures like the seminal vesicles or bladder neck, causing noticeable urinary and reproductive symptoms. While stage 3 prostate cancer is serious, it is still treatable with a combination of therapies aimed at controlling tumor growth and preventing further spread.
Types
Prostate cancer can vary depending on its growth pattern and aggressiveness:
- Adenocarcinoma: The most common type, originating from gland cells in the prostate.
- Ductal adenocarcinoma: A rarer, more aggressive subtype.
- Neuroendocrine tumors and small cell carcinomas: Uncommon types that tend to spread quickly and require specialized treatment approaches.
Understanding the type of prostate cancer helps doctors determine the best treatment plan for stage 3 cases.
Causes and Risk Factors
While the exact cause of prostate cancer remains unknown, several risk factors increase the likelihood of developing the disease:
- Age: Most cases occur in men over 50.
- Family history: Having a father or brother with prostate cancer raises risk.
- Genetics: BRCA1, BRCA2, and other gene mutations may contribute.
- Race and ethnicity: African American men have a higher risk and tend to develop more aggressive cancers.
- Diet and lifestyle: High-fat diets, obesity, and lack of exercise can increase risk.
- Hormonal factors: High testosterone levels may promote cancer growth.
Symptoms and Early Warning Signs
Recognizing stage 3 prostate cancer symptoms can be life-saving. Common signs include:
- Frequent urination, especially at night (nocturia)
- Difficulty starting or stopping urination
- Weak or interrupted urine flow
- Blood in urine or semen
- Pelvic or lower back pain
- Painful ejaculation or discomfort during urination
- Erectile dysfunction
At stage 3, symptoms may become more severe due to the tumor pressing on nearby tissues. Persistent pain in the hips or thighs and urinary obstruction are also possible indicators.
Diagnosis
Diagnosing stage 3 prostate cancer involves several steps:
- Digital Rectal Exam (DRE) to feel for abnormalities.
- Prostate-Specific Antigen (PSA) test to measure PSA levels in the blood.
- MRI or CT scans to assess tumor spread beyond the prostate.
- Biopsy to confirm the presence and grade of cancer cells.
- Bone scans to detect possible bone involvement.
Accurate staging is crucial for choosing the most effective treatment plan.
Treatment Options
Treatment for stage 3 prostate cancer often combines multiple approaches:
- Radiation therapy: Targets and destroys cancer cells while preserving healthy tissue.
- Hormone therapy (Androgen Deprivation Therapy): Reduces testosterone, slowing cancer growth.
- Surgery (Radical Prostatectomy): Removes the prostate gland and affected tissues.
- Chemotherapy: Used when cancer is aggressive or resistant to hormone therapy.
- Targeted and immunotherapy: Emerging treatments that attack cancer cells more precisely.
The treatment choice depends on cancer aggressiveness, patient health, and preferences.
Prevention and Lifestyle Recommendations
While not all prostate cancers are preventable, certain habits may lower risk:
- Maintain a balanced diet rich in fruits, vegetables, and omega-3 fatty acids.
- Exercise regularly to maintain a healthy weight.
- Limit red and processed meats and reduce dairy intake.
- Avoid smoking and excessive alcohol consumption.
- Get regular checkups if you have a family history of prostate cancer.
Adopting a healthy lifestyle supports treatment recovery and reduces recurrence risk.
Prognosis and Survival Rates
The prognosis for stage 3 prostate cancer varies depending on tumor aggressiveness and treatment response. According to clinical studies, the 5-year survival rate remains high—around 85–95%—when treated promptly and effectively. Early detection and consistent follow-up care significantly improve long-term outcomes.
Latest Research and Innovations
Recent advancements in prostate cancer treatment include:
- Genomic testing to personalize treatment based on genetic mutations.
- Proton beam therapy for more precise radiation delivery.
- Advanced imaging technologies like PSMA PET scans for early metastasis detection.
- New hormone therapies that target androgen receptors more effectively.
Ongoing research continues to enhance survival rates and quality of life for patients with stage 3 prostate cancer.
Coping and Support for Patients
Living with stage 3 prostate cancer can be emotionally and physically challenging. Support is available through:
- Counseling and therapy to manage stress and anxiety.
- Support groups where patients share experiences and coping strategies.
- Nutrition and fitness programs tailored for cancer patients.
- Family involvement in care decisions and emotional support.
A strong support network and positive outlook play a major role in improving quality of life during and after treatment.
Conclusion
Stage 3 prostate cancer symptoms can be alarming, but with timely diagnosis and effective treatment, many men continue to lead fulfilling lives. Understanding risk factors, recognizing warning signs, and following medical guidance can make a significant difference in outcomes.
Early detection remains the most powerful weapon against prostate cancer—regular screenings and healthy lifestyle choices are key to prevention and long-term wellness.
FAQ
1. What are the first signs of stage 3 prostate cancer?
Frequent urination, difficulty urinating, and pelvic pain are common early indicators.
2. Can stage 3 prostate cancer be cured?
While complete cure is less likely than in early stages, effective treatment can control and manage the disease for many years.
3. How fast does stage 3 prostate cancer spread?
It varies by individual; aggressive forms may spread quickly, while slower-growing ones can remain localized for years.
4. What is the life expectancy with stage 3 prostate cancer?
Many patients live 10 years or longer with proper treatment and follow-up care.
5. How often should I get screened for prostate cancer?
Men over 50 (or over 40 with a family history) should discuss annual PSA testing with their doctor.