Bladder cancer is a serious health concern affecting thousands of individuals worldwide each year. Among the available treatment options, Bacillus Calmette-Guérin (BCG) therapy has become a cornerstone for managing non-muscle invasive bladder cancer (NMIBC). Patients and families often seek reliable information about the effectiveness of this treatment, particularly regarding the BCG treatment for bladder cancer success rate.
Understanding the potential outcomes of BCG therapy is essential for making informed decisions. This article explores the definition, causes, risk factors, symptoms, diagnostic methods, treatment options, and long-term outlook for bladder cancer, with a focus on how successful BCG treatment can be in preventing recurrence and progression.
Definition and Overview
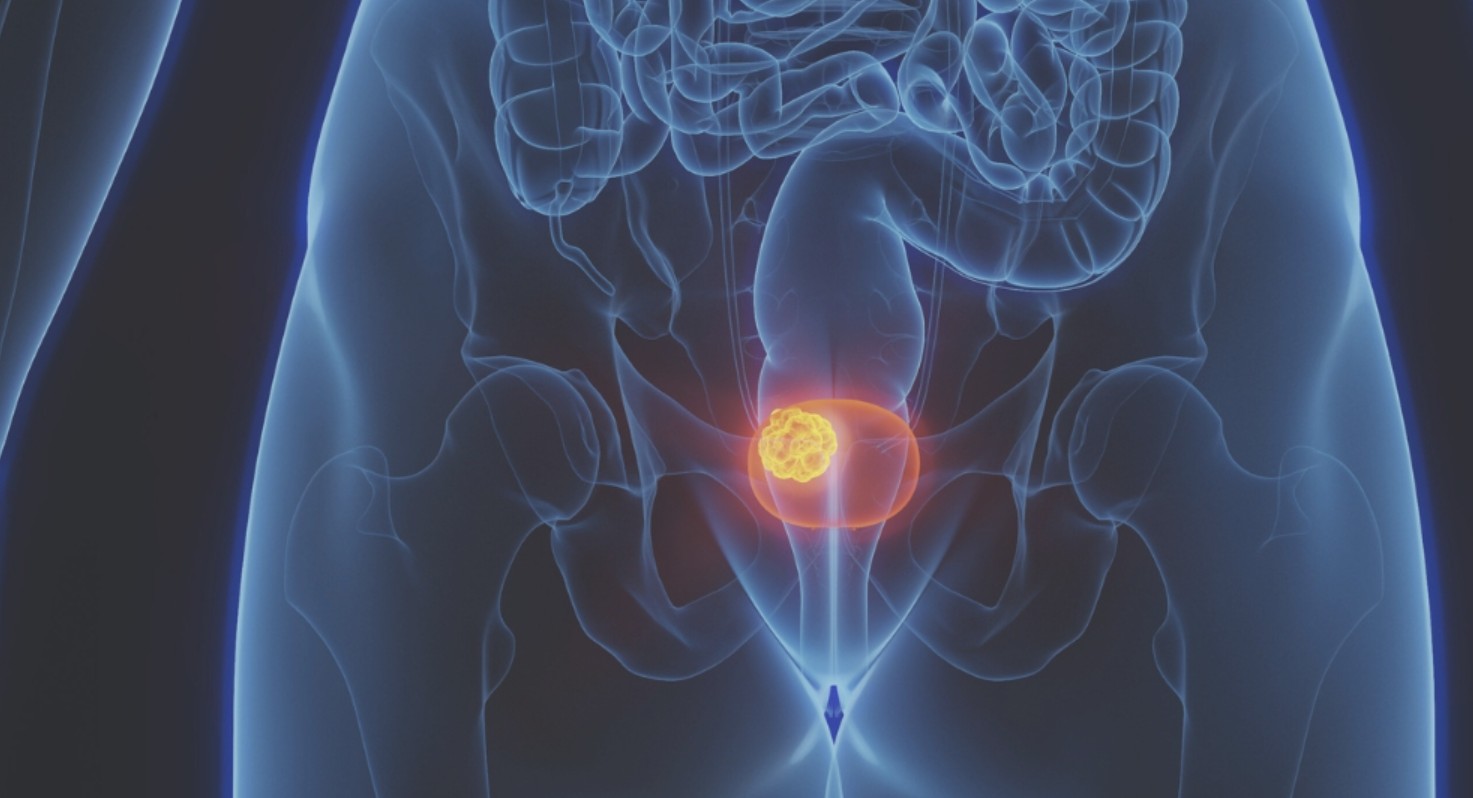
Bladder cancer occurs when abnormal cells in the bladder grow uncontrollably, forming tumors. The most common type is urothelial carcinoma, which begins in the bladder’s inner lining. BCG treatment is an immunotherapy that uses a weakened strain of Mycobacterium bovis to stimulate the body’s immune system and attack cancer cells. It is primarily recommended for patients with early-stage bladder cancer to reduce recurrence and progression.
Types
There are several types of bladder cancer, including:
- Urothelial carcinoma (transitional cell carcinoma): The most common form.
- Squamous cell carcinoma: Linked to chronic irritation or infection.
- Adenocarcinoma: Rare, arising from glandular cells in the bladder.
BCG therapy is particularly effective in treating non-muscle invasive urothelial carcinoma, especially carcinoma in situ (CIS).
Causes and Risk Factors
Bladder cancer risk factors include:
- Smoking: The leading cause, contributing to nearly half of all cases.
- Chemical exposure: Contact with industrial chemicals like arsenic and dyes.
- Chronic bladder inflammation: From infections or long-term catheter use.
- Age and gender: More common in older men.
- Family history and genetics: Certain inherited conditions raise the risk.
Symptoms and Early Warning Signs
Early detection plays a major role in improving outcomes. Symptoms may include:
- Blood in urine (hematuria)
- Frequent urination or urgency
- Pain during urination
- Pelvic or back pain in advanced stages
Recognizing these warning signs can lead to earlier diagnosis and timely initiation of treatments like BCG therapy.
Diagnosis
Bladder cancer is diagnosed using multiple approaches:
- Urinalysis and urine cytology: To detect cancer cells in urine.
- Cystoscopy: A small camera inserted into the bladder for direct visualization.
- Biopsy: Tissue samples confirm the presence of cancer.
- Imaging tests: CT scans, MRIs, or ultrasounds to assess cancer spread.
Treatment Options
Treatment varies depending on the stage and grade of the cancer:
- Surgery: Transurethral resection of bladder tumor (TURBT) for early-stage cancers.
- BCG therapy: Administered directly into the bladder via catheter, it is one of the most effective immunotherapy options.
- Chemotherapy: Used intravesically or systemically for advanced disease.
- Radiation therapy: Less common but considered in certain cases.
- Targeted therapy and immunotherapy drugs: Emerging options for advanced stages.
Prevention and Lifestyle Recommendations
While bladder cancer cannot always be prevented, steps can reduce risk:
- Avoid smoking and secondhand smoke.
- Stay hydrated to help flush the bladder.
- Minimize exposure to harmful workplace chemicals.
- Maintain a balanced diet rich in fruits and vegetables.
- Attend regular medical checkups, especially for those at high risk.
Prognosis and Survival Rates
The BCG treatment for bladder cancer success rate is generally favorable, particularly for non-muscle invasive bladder cancer. Studies show that BCG therapy can reduce recurrence rates by 30–40% and lower progression risks significantly. Five-year survival rates for NMIBC patients receiving BCG are high, often exceeding 70–80%, depending on tumor grade and patient health. However, results vary, and some patients may not respond to BCG, requiring alternative therapies.
Latest Research and Innovations
Recent innovations are focused on improving BCG treatment effectiveness and overcoming shortages. Researchers are exploring combination therapies that use BCG alongside immune checkpoint inhibitors. Novel delivery methods and genetic profiling are also helping tailor treatment to individual patients, potentially boosting success rates even further.
Coping and Support for Patients
Bladder cancer treatment can be emotionally and physically challenging. Patients benefit from:
- Support groups: Sharing experiences with others facing similar challenges.
- Counseling services: Addressing anxiety, depression, or fear of recurrence.
- Patient education: Understanding treatment options improves confidence in care decisions.
- Family support: Loved ones play a crucial role in motivation and recovery.
Conclusion
BCG therapy remains one of the most effective treatments for non-muscle invasive bladder cancer. The BCG treatment for bladder cancer success rate highlights its role in preventing recurrence and progression, offering hope to patients diagnosed at earlier stages. While not effective for everyone, ongoing research continues to improve its outcomes and expand future possibilities.
For patients and caregivers, understanding treatment success rates, risks, and coping strategies is vital. With the right combination of medical care, lifestyle adjustments, and emotional support, many individuals can achieve a better quality of life and improved survival outcomes after bladder cancer treatment.