HPV-related throat cancer is one of the fastest-growing types of cancer linked to the human papillomavirus (HPV). In recent years, medical research has shown that HPV is not only a common cause of cervical cancer but also plays a major role in oropharyngeal cancers, which affect the throat, tonsils, and base of the tongue. Understanding the condition, its symptoms, and treatment options is crucial for improving survival outcomes.
One of the most frequently asked questions is about the HPV throat cancer survival rate. This article explores the definition, risk factors, symptoms, diagnosis, treatments, and prevention strategies. It also discusses prognosis, the latest research, and ways patients can cope with the physical and emotional challenges of the disease.
Definition and Overview
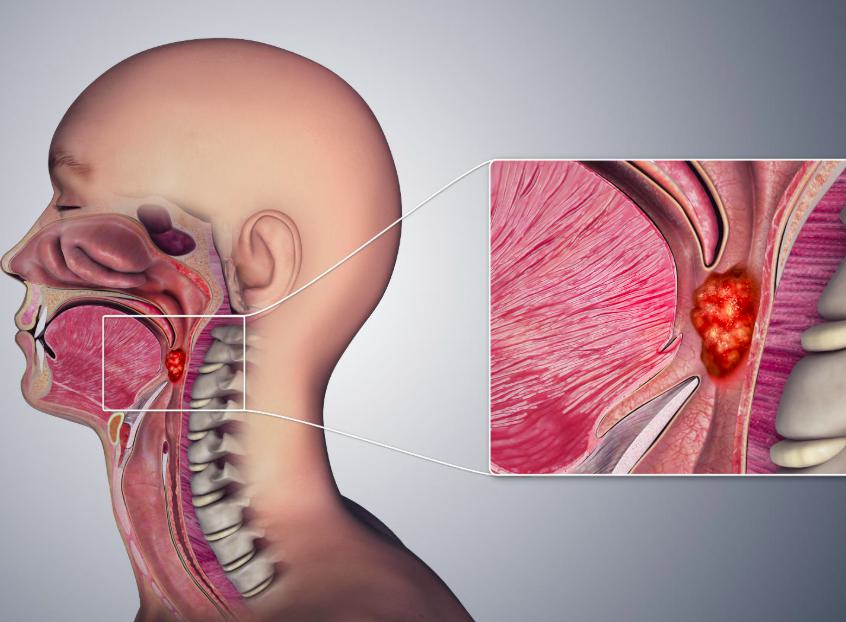
HPV throat cancer, medically known as HPV-positive oropharyngeal squamous cell carcinoma, develops in the throat tissues infected by certain strains of HPV, especially HPV-16. Unlike traditional throat cancers often caused by tobacco and alcohol, HPV-related cancers tend to affect younger, otherwise healthy individuals.
This type of cancer is now more common than cervical cancer in many countries, particularly among men. The HPV throat cancer survival rate is generally more favorable compared to non-HPV throat cancers, thanks to better responsiveness to treatment.
Types
HPV-related throat cancer primarily falls under oropharyngeal cancers, including:
- Tonsil cancer
- Base of tongue cancer
- Soft palate cancer
- Side and back walls of the throat
Each type may present differently but shares a strong association with HPV infection.
Causes and Risk Factors
The main cause of HPV throat cancer is infection with high-risk strains of the human papillomavirus, particularly HPV-16. Risk factors include:
- Multiple oral sex partners
- Weakened immune system
- Male gender (men are more likely to develop HPV throat cancer)
- Age between 40 and 60 years
Unlike traditional risk factors for head and neck cancers, smoking and alcohol play a less significant role in HPV-related cases.
Symptoms and Early Warning Signs
HPV throat cancer often develops silently. Common symptoms include:
- Persistent sore throat
- Difficulty swallowing
- Swollen lymph nodes in the neck
- Ear pain without infection
- Hoarseness or voice changes
- Unexplained weight loss
Because early signs may seem mild, many cases are diagnosed at advanced stages.
Diagnosis
Diagnosis involves several steps:
- Medical history and physical exam
- Imaging tests (CT, MRI, PET scans)
- Biopsy of affected tissue
- HPV testing on cancer cells
Early and accurate diagnosis is essential for treatment planning and improving the HPV throat cancer survival rate.
Treatment Options
Treatment for HPV throat cancer may include:
- Radiation therapy: Often effective for localized cancers.
- Chemotherapy: Used in combination with radiation for advanced cases.
- Surgery: Minimally invasive techniques, such as transoral robotic surgery (TORS), may be used.
- Targeted therapy and immunotherapy: Newer approaches designed to attack cancer cells more precisely.
Because HPV-positive cancers respond better to treatment, survival outcomes are typically better compared to non-HPV cancers.
Prevention and Lifestyle Recommendations
Prevention strategies include:
- HPV vaccination: Highly effective in reducing the risk of HPV-related cancers.
- Safe sexual practices: Using protection and limiting sexual partners.
- Regular health checkups: For early detection of abnormalities.
- Healthy lifestyle: Avoiding smoking, reducing alcohol consumption, and maintaining a strong immune system.
Prognosis and Survival Rates
The HPV throat cancer survival rate is significantly higher than that of non-HPV throat cancers. According to research:
- The 5-year survival rate for HPV-positive throat cancer is around 80–90%.
- For non-HPV throat cancer, survival rates are typically lower, around 50–60%.
Factors influencing prognosis include the stage of cancer, age, overall health, and response to treatment.
Latest Research and Innovations
Recent studies are focused on:
- De-escalation therapies to reduce treatment side effects while maintaining survival rates.
- Immunotherapy advancements that help the body’s immune system fight cancer.
- Improved screening methods for earlier detection.
These innovations continue to enhance treatment outcomes and the quality of life for patients.
Coping and Support for Patients
Living with HPV throat cancer involves both medical and emotional challenges. Patients benefit from:
- Support groups and counseling
- Nutritional guidance to maintain strength during treatment
- Speech and swallowing therapy when needed
- Family and caregiver involvement for emotional support
Conclusion
HPV throat cancer is increasingly common but carries a more favorable outlook compared to traditional throat cancers. With proper diagnosis, effective treatment, and preventive measures like HPV vaccination, the HPV throat cancer survival rate continues to improve. Staying informed and proactive plays a vital role in managing risks and enhancing quality of life.
FAQ
1. What is the average HPV throat cancer survival rate?
The 5-year survival rate for HPV-positive throat cancer is approximately 80–90%, much higher than non-HPV cases.
2. Can HPV throat cancer be cured?
Yes, many cases can be cured, especially when diagnosed early and treated effectively.
3. Who is most at risk for HPV throat cancer?
Men between ages 40 and 60 with multiple oral sex partners are at the highest risk.
4. How does HPV throat cancer differ from non-HPV throat cancer?
HPV-related cases respond better to treatment and have higher survival rates compared to cancers caused by smoking and alcohol.
5. Can HPV vaccination prevent throat cancer?
Yes, HPV vaccines significantly reduce the risk of developing HPV-related throat cancers when given before exposure to the virus.